Forensic psychiatrist Rees Tapsell tells the story of “Tama”, who killed his aunt in a psychotic episode, and was referred to a kaupapa Māori rehabilitation unit.
As a Māori forensic psychiatrist, I have been responsible for the treatment and rehabilitation of Māori who suffer mental illness and have committed violent offences while mentally unwell. In my experience, successful kaupapa Māori rehabilitation units for such offenders are founded on five key factors:
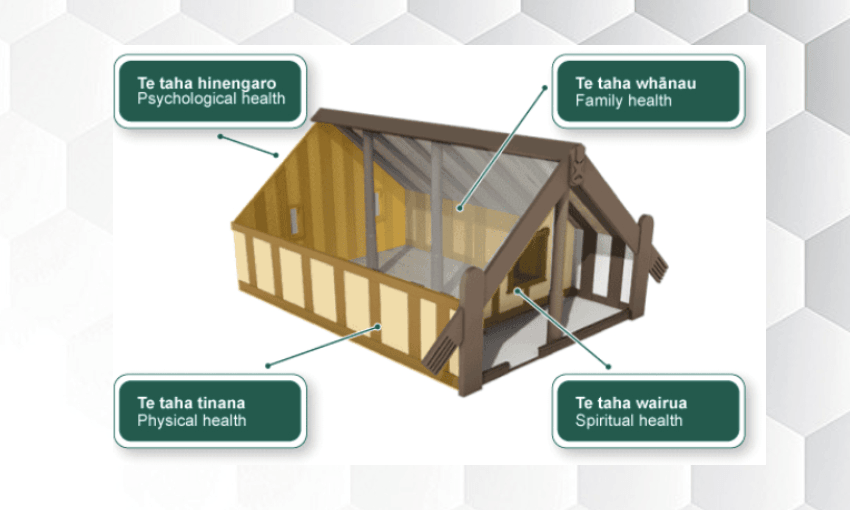
- They are underpinned by Māori principles and a model of care that is based on Māori kaupapa and tikanga.
- They offer a healing environment that facilitates a culturally informed model of care. They also have a central focus for cultural activities; a whare is ideal.
- Whether owned by a mainstream government provider or a Māori non-government organisation, there is a clear and unrelenting commitment to a model that integrates best practice (Māori) cultural and clinical (forensic) interventions.
- The leaders of these units have dual clinical and cultural competencies.
- Units are well staffed by committed people who, where possible, are Māori.
These principles come to life with a case study. In the following story of “Tama”, names and other key details have been amended and to a large extent the case is an amalgam of dozens that I have experienced as a forensic psychiatrist. But it serves to illustrate key challenges, as well as opportunities and the potential for health gains.
*
Tama is a 25-year-old, single, Māori male who was admitted to a forensic mental health service, having been found not guilty by reason of insanity on a charge of murder, relating to an incident in which he stabbed his maternal aunt while acutely psychotic. His aunt died at the scene.
Tama was born into a gang family and had a disruptive development, characterised by conduct problems, early alcohol and cannabis abuse, frequent violence and anti-social behaviour. The family had some understanding of te ao Māori but little knowledge of te reo or tikanga Māori. Tama lived with his mother on the periphery of a gang through most of his development. While of average intelligence, he was expelled from school at the age of 16 and had never had a job. Tama developed a psychotic disorder at the age of 23, but neither he nor his father accepted that he had an illness or required treatment. Tama’s mother was very close to her son, whom she described as a sensitive and artistic boy. She had left Tama’s father, in very traumatic circumstances, two years before the incident. Tama and his mother were living with his aunt (the victim) and her family at the time of the incident, having recently shifted back to the region of Tama’s birth. Tama’s mother had unsuccessfully encouraged him to seek treatment.
The shock of the incident convinced Tama’s father that Tama was ill. Following the incident, Tama remained psychotic, requiring treatment with Clozapine. He was confused, detached and lacked insight and proved very difficult to engage with. After 18 months in a mainstream secure forensic environment, Tama was referred to a kaupapa Māori rehabilitation unit within the same service for ongoing rehabilitation.
Although his whānau were supportive of his admission to this unit, at the time of his referral Tama was ambivalent. At his initial assessment by the unit manager (Māori) and me, Tama described feeling lost and did not see a future for himself. He was suspicious and discussed a number of psychotic themes rather than his own situation or what had happened to bring him into hospital. He felt as though his whānau were angry and disappointed with him about what had happened, and although not obviously depressed, he remained apathetic about the future.
Our assessment occurred over three sessions of approximately 90 minutes each. The first session was with Tama and his mother; the second involved his father, who attended reluctantly; and the last was with Tama alone. All sessions were attended by kaumātua and were preceded by karakia and whakawhanaungatanga.
While neither Tama nor his family spoke Māori or were fully competent in the formal Māori process, the opportunity to engage with the treatment team as equals and to establish connections as whanaunga contributed significantly to establishing a degree of rapport. Even though Tama remained somewhat ambivalent towards the unit, his levels of suspiciousness through the assessment process visibly lessened, as did his tendency to resort to senseless psychotic themes rather than answer questions that were put to him or to discuss himself.
Tama felt frightened, confused and ashamed of the pain he had caused his family. He outwardly presented himself as a strong young man, but he was very sensitive and unsure of who he was in the world, and he felt very angry and resistant to mainstream approaches to his illness. While not fully understanding the difference of a kaupapa Māori approach, it was clear that both Tama and his family appreciated that this kind of care better reflected them and their world view.
*
Tama remained quiet and reserved initially but steadily warmed to the unit and its residents. He took some time to settle into the community but began to become comfortable in this environment and increasingly participated in programmes. He enjoyed te reo lessons and kapa haka and displayed a particular interest in knowing more about his whakapapa and tīpuna.
Tama warmed to a number of younger Māori staff, and we capitalised on this to encourage him to take on a role within the community as kaikarakia at meals. He also excelled in the artistic programmes and gained a real sense of enjoyment and pride in carving class. As Tama further engaged with the programmes and with whānau within the unit, he became much more accessible and much less preoccupied with the psychotic content of his thinking.
Over time, Tama began to spend regular time with the unit kaumātua, fine-tuning his knowledge of whakapapa. It was in these sessions that discussions began around his violence and his substance misuse and its effect on his whakapapa going forward. Tama displayed the first signs of wanting to discuss ways in which he could change his life and began to think much more positively about his future.
Ward rounds in the unit involved significant input from patients and their whānau, where possible and appropriate. In the early days, Tama would contribute very little, but as his self-esteem improved and his outlook became more positive, he began to take charge of his clinical review meeting and collaboratively plan for his future in a much more reasonable and appropriate way. In particular, Tama and his family were more accepting and understanding of situations in which they did not immediately receive what they wanted (for instance, where legal status prohibited a particular activity) and displayed more patience.
There were times, particularly at the initial stages of treatment, where Tama displayed unacceptable or disruptive behaviour within the unit. This was addressed within the safety of the tikanga of the unit. As part of this, formal community meetings were organised where each member of the unit had an opportunity to participate in discussions about the transgression and the eventual consequences of it. Tama’s mother noted that this was the first time Tama had ever accepted responsibility for his actions. Gradually, Tama was given approval for leave from the unit in increasing amounts. On some occasions minor setbacks, such as drinking alcohol, occurred, but these were effectively managed by Tama being made accountable to both the community and the Ministry of Health and by a temporary withdrawal of leave privileges.
In time, it was decided that Tama should travel home to his aunt’s marae in rural Waikato so he could visit his aunt’s grave and meet with members of his aunt’s family. Tama was very anxious about this and required significant support from the unit. Ultimately, however, this visit went well. Tama visited his aunt’s grave and became very emotional as he expressed his remorse for what he had done. While most of his family accepted his apology, several did not, and they voiced their distress. Tama was able to navigate this situation well with no anger or deterioration in his mental state and further showed his capacity to accept this without responding. Later, he acknowledged that the support he had had from kaumātua and unit staff had been important in being able to do this.
Tama participated well in a variety of other programmes. He warmed particularly to an anti-violence programme that was facilitated by a young Māori carver who used historical stories to promote these messages. Tama was given the role of kaikōrero for the unit, speaking on behalf of the residents during formal processes.
Tama’s relationship with his mother strengthened, and she was very involved in his rehabilitation. His father remained more distant yet supportive, attending several formal events within the unit and supporting friends during similar marae visits. While his father remained an active gang member and continued to smoke cannabis heavily, he agreed not to wear his gang patch in the unit, accepted that alcohol and drug use was not consistent with his son’s rehabilitation and agreed to ensure that others would not provide Tama with alcohol or drugs when he was in his care.
Tama remained at the unit for 18 months before being referred to a kaupapa Māori supervised residential home with follow-up provided by staff from the forensic mental health service. In preparation for this transition, he engaged with a Māori community care worker (nurse), with the interventions shifting gradually from the unit to community-based activities. In contrast to the unit, the cultural and clinical interventions were provided by different teams. In spite of this, Tama remained engaged with each, and both he and his whānau accepted that he would need to spend some time in a supervised accommodation setting before returning home.
Throughout Tama’s stay at the unit, my role as his psychiatrist and the clinical leader in the unit was to ensure that he received the best possible biological, psychological and socio-cultural management while modelling a commitment to, and maintaining involvement in, all critical cultural activities. This involved situations in which I would sometimes identify the need to prioritise a cultural intervention or imperative over a clinical one or vice versa. At times, this caused disappointment for Tama and his whānau, but I was always confident of the sound rationale for the decision and used these situations as opportunities for learning.
Throughout Tama’s stay, we gathered objective data on his progress. We scored him on objective scales of his mental state, general rehabilitative progress and risk. In addition, we spent considerable time developing an internal tool for assessing cultural competency as a proxy for the development of cultural identity. Despite some residual psychosis, Tama showed objective and progressive improvements in his general mental state and functioning and a corresponding reduction in his risk scores.
As Tama began to spend more and more time in the community, with his family and engaged in community activities, his focus shifted to his community placement and community activities. He developed the longer-term aim of becoming a graphic artist and decided that he would like to return to Hamilton to be closer to his mother and more pro-social members of his whānau.
The poroporoaki for Tama was a celebration of his success. It was attended by members of his whānau, his community team and all staff and other patients from the unit. It was an emotional process in which Tama took an active part, speaking candidly about his experiences moving through the forensic service and identifying the importance of the unit and its approach to engaging with him.
Tama left the unit after 18 months as a resident and nearly three years within the service in total. He continues to visit the unit for important events. While he had periods where he required additional support from staff at the unit, he was not readmitted. Approximately five years after being found not guilty by reason of insanity, he was reclassified as a patient subject to a civil order and transferred to the Waikato.
*
Having worked with Māori in forensic mental health services in a range of different services and contexts, I’m left with the following conclusions.
First, my practice-based evidence is that culturally inspired or integrated interventions offer a successful approach for many Māori, and their whānau, who have initially struggled to see the value of a mainstream approach to treatment and rehabilitation.
Second, irrespective of whether such an approach is provided by a mainstream government provider or a non-government Māori provider, the importance of having staff who maintain dual competence within both the Māori and clinical worlds and a commitment to the model of care cannot be overstated. This requires an explicit statement of the model of care and its underpinning principles, careful selection of staff (based on their personal values, level of competence and commitment), strong leadership within the unit and clear support for it by the wider forensic mental health establishment.
Third, although there is widespread support for this type of unit, it makes up only one part of a patient’s journey through wider forensic mental health services. There is the opportunity to extend this model of care across all aspects of the service, beginning in prison and moving through the acute and secure, rehabilitation and community components.
Finally, if we are to accept that the concept of dual competence, cultural and clinical, has validity as a perquisite for the provision of mental health services for Māori, then we should actively explore opportunities to develop training approaches that explicitly incorporate them into one integrated discipline.
This edited extract is taken from Maea te Toi Ora: Māori Health Transformations, by Rees Tapsell, Te Kani Kingi, Mason Durie, Hinemoa Elder, Mark Lawrence and Simon Bennet (Huia Publishers, $45), available at Unity Books.