In 2019, an Auckland woman woke up from surgery to find that she had undergone a treatment she didn’t consent to. She tells Alex Casey about her experience.
From her very first period at the age of 14, Laura experienced “debilitating” levels of pain that forced her to withdraw from many parts of her life. “I stopped doing things. I quit Taekwondo, I stopped all my sports because I was just in so much pain,” she says, now 29 years-old. “I tried going to a gynaecologist and got the same old story that a lot of people with endometriosis have, where they say ‘oh, you’re too young to have it’.”
The worst bouts of pain would leave her curled up on the floor, unable to move. “I remember being in bed being in so much pain that I couldn’t even reach for painkillers. It’s not just a bad period. It’s actually debilitating, even for the most resilient person.”
When she entered the workforce, she worried about how many sick days she needed to take. “For a long time I had that fear of being treated differently or being passed over for a promotion,” she says. It would take more than a decade for Laura to be diagnosed with endometriosis, discovered during a laparoscopy for a cyst in 2019. “It was this mixed feeling of validation, but also this feeling of, ‘oh my gosh, I’ve got this lifelong illness that doesn’t have a cure’.”
Laura is one of the 120,000 people in New Zealand affected by endometriosis, an inflammatory disease that causes the endometrium (uterus lining) to grow outside of the uterus. Symptoms can include period pain, bowel problems, abnormal bleeding and fertility issues. There is currently no cure for endometriosis, with one in 10 menstruating New Zealanders forced to manage their ongoing symptoms through pain relief, hormonal treatments and surgeries.
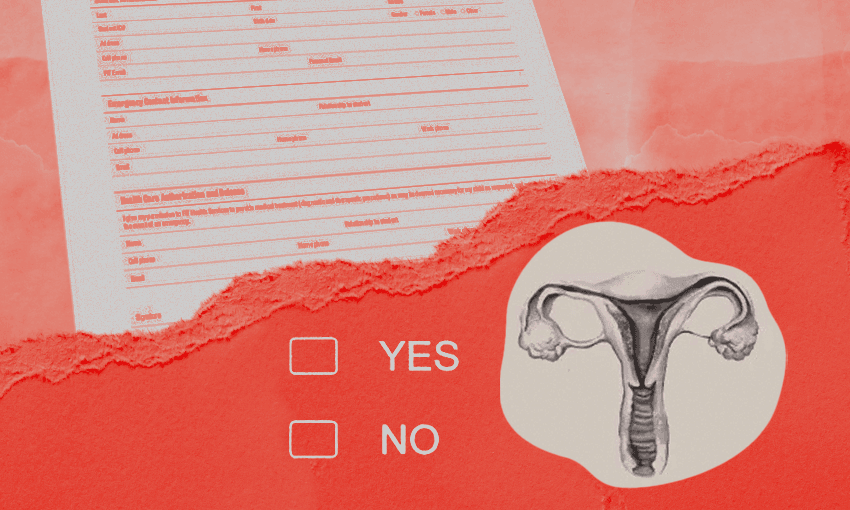
After she was diagnosed in March 2019, Laura went on a waitlist for surgery to remove her endometriosis tissue. According to Australian and New Zealand guidelines, the most effective methods in the surgical treatment of endometriosis are excision (cutting out the tissue) or ablation (destroying the tissue through burning). After discussions with her surgeon and her own extensive research, Laura decided she wanted to receive excision instead of ablation, and “felt really comfortable” with the surgeon and their conversations.
When she arrived on the day of surgery in September 2019 to find that her surgeon was off sick, Laura ensured she made clear on her form that she was consenting to excision only. But waking up after the procedure “full of drugs and all over the place”, she was informed that her fill-in surgeon had used both excision and ablation during the procedure. “It was such a shock,” she says. “To wake up and be told that something’s happened that you didn’t want to happen feels like your agency is taken away.”
Laura says that discovering she had received the treatment was yet “another blow” after years of feeling dismissed by the health system, and being told that her pain was “normal” or that she just “needs to get pregnant” to fix it. “There’s such a psychological element to endometriosis, because you’re told from such a young age that you’re weak, and that everyone feels this pain and you’re just being a baby about it,” she says. “That feeling of dismissal is carried through your whole experience with healthcare professionals.”
Following the surgery, her pain worsened. “I was getting these cramps that left me on the floor,” she says. “I remember going into the office and being in so much pain that I had to go home, and that’s a really hard thing to communicate to your employer when you’re trying to be this high-achieving employee.” She recalls being “distressed” in her follow-up appointment with the surgeon, and again felt dismissed when she raised concerns about receiving ablation treatment that she did not want.
“It felt like they were not taking responsibility for the fact that they had performed a surgery on me that I had made very clear I was not comfortable with being performed,” she says.
It was only when she saw an article about a similar case from 2015, in which a woman woke up feeling “shocked, upset and alone” after receiving ablation treatment, despite only consenting to excision, that Laura realised she wasn’t alone. In 2020, the Health and Disability Commissioner found that the woman’s case was a breach of Code of Health and Disability Services Consumers’ Rights. “I read that and just thought ‘oh, my gosh, this is exactly my experience’.”
The story inspired Laura to make a complaint of her own to the HDC, who last month found that her specialist breached the Code of Health and Disability Services Consumers’ Rights. Under the code, “consumers have the right to the information that they need to make an informed choice or give consent”, and “services may be provided to a consumer only if that consumer makes an informed choice and gives informed consent.”
As part of the investigation, the surgeon explained that “99% of the operation proceeded by way of excision in accordance with [Laura’s] wishes. When I found a small ‘pea’ sized lesion which [was] close to the bowel I removed this by way of ablation.” An independent gynecologist offering advice on the investigation noted that “it would be inappropriate for a surgeon to undertake excision on bowel where excision would run a high risk of perforation.”
The surgeon also disputed the lack of consent, saying “must I proceed to discuss a list of possible eventualities potentially leading to patient confusion to the extent that they no longer have any confidence or understanding about which procedure they are consenting for?”
In its findings, the HDC accepted that the surgeon had approached the lesion in a medically-appropriate way, but added that the appropriateness of the surgical option was not the central issue. “Rather, the concern is that having had the surgical approaches discussed with her, [Laura] expressly indicated that she did not want ablation — as was her right.” The Commissioner found that Laura had clearly communicated her choice, and a breach of the Code was determined in regards to her right to choice and consent.
“It feels really validating – I had a big cry when it came through,” says Laura. “To have it acknowledged that my experience shouldn’t have been like this makes such a big difference.”
Now living in the UK, Laura has since received excision treatment through the NHS and has found “quite a significant” reduction in her pain, managing most of the time with over the counter pain medication and the flexibility to work from home. “It still impacts me on a monthly basis, but not to the extent that I’m being hospitalised for the pain,” she says. “But I’m going to be fighting for this my whole life – not just fighting for myself, but fighting for other people.”
In speaking up about her own experiences, Laura hopes to raise more awareness around the realities of living with endometriosis. “Anyone that’s navigated the health system as a female, knows it is like hitting your head against the wall,” she says. “I’m quite strong-willed in terms of standing up for myself in the health system. I did a psychology degree, I have a background that so many people won’t have, and I still found it so difficult to stick up for myself.”
Her advice to other people in her position is to not just be your own advocate, but find other people who can support you. “I would go to the appointments by myself, feel really strong beforehand, but as soon as I’d sit in that chair I’d get emotional and I wouldn’t be able to fight for myself in that specific situation,” she says. “Whereas if I had someone that I trusted with me, they would be able to support me through it a bit more.”
Bringing in written notes is another good way to ensure that the right information is being communicated, says Laura, as is ensuring that your doctor is including everything in their notes. In her case, her request for excision only was not in the written notes that were handed over to the new surgeon. “It really helps you not just keep a record of it, but also advocate for yourself because the doctor then also has to take ownership of those decisions.”
Whether it is the final year medical student who told her he had never heard of endometriosis, or her friend still struggling to get a diagnosis after 10 years of excruciating pain, Laura says there’s clearly still a lot more work to be done around endometriosis education both here and abroad. Even during her most recent smear test in the UK, she gave the women’s health nurse a heads up that she has endometriosis, and sometimes finds the procedure painful.
The nurse looked up at her, confused: “what is endometriosis?”