On Monday we published a piece in which midwives spoke out. They talked about how exhausted they are, how they’re underpaid and overworked and underappreciated. Today we share the responses we received from politicians, and from NZ’s main midwives organisation.
Following Monday’s story, we heard again and again from readers who were shocked by the way midwives were feeling. All agreed that to something must be done to address staff shortages and the high turnover rate of midwives. But what about politicians? Here’s what they think.
For balance, we approached the Ministry of Health and Minister for Health Jonathan Coleman. Mr Coleman did not respond.
A Ministry of Health spokesperson:
The Ministry recognises the very important work of midwives in producing good outcomes for mothers and babies in both DHB maternity units and in LMC work. The Ministry is reliant on DHBs to ensure that the work environment for midwives employed there is safe and supportive of the work they are there to do.
It’s important midwives voices and work experiences are heard by the Ministry, and this occurs regularly, primarily through a number of important working groups including the Midwifery Strategic Advisory Group and the National Maternity Monitoring Group.
Currently, there are 1,377 midwives working in DHBs across the country and a record 2,980 midwives working in our health system.
The Ministry is aware that some urban DHBs are experiencing difficulty recruiting sufficient midwives. The Ministry is working with DHBs and other groups such as the NZ College of Midwives and the Midwifery Council to understand the issue so a solution can be found.
The Ministry supports new graduate midwives through the first year of practice programme, the voluntary bonding scheme, as well as locum support for rural midwives.
Health Workforce New Zealand’s (HWNZ) Midwifery Strategic Advisory Group has identified the DHB midwifery workforce issues as a priority. The Ministry of Health is working with the Tertiary Education Commission to understand where midwifery students are coming from and therefore where they are likely to work.
The Ministry has recently signed a memorandum of understanding with the Midwifery Council for sharing data about the midwifery workforce that will enable detailed regional modelling of the midwifery workforce. Both these activities will contribute to possible solutions for the problem with the distribution of the midwifery workforce.
Labour Party deputy leader Jacinda Adern:
Its hard to know what to say without sounding trite. Midwifery is such a hard and demanding profession, so I feel anything I say would understate that. But we know that health is hugely underfunded at present and as a result DHBs cannot ensure safe staffing (sufficient number of nurses on wards etc.) There should be midwives on wards overnight and in the weekends to support mothers. And enough of them, but there’s not.
Everyone knows that you can’t plan for when a baby is born but we staff maternity facilities as if babies are born 9 to 5 Monday to Friday. Over 50% of babies are born at night, after hours or at weekends when staffing is minimal. But like I say, this isn’t something that we’re debating on paper – my friend recently experienced it first hand. Funding health properly would be a great start, recognising the importance of our midwifes would be too.
Labour health spokesperson Dr David Clark:
As a result of the coverage, Dr David Clark asked the Minister for Health Jonathan Coleman “is he confident that new mothers are being supported in public hospitals”.
Nicky Wagner said on behalf of Mr Coleman “yes, absolutely. Our Government prioritises the health of mothers and babies, but as always in health, we are keen to continue to improve our services, to meet the expectations of every new mother.”
Dr Clark then asked: Is he confident that the district health boards (DHBs) have enough funding to ensure that there are enough midwives rostered on in the weekends or after hours in hospitals, when new mothers like Mary-Lou Harris, who experienced complications at birth, are left unsupported overnight and feel unsafe because nurses are too overstretched on wards?
Ms Wagner: Yes, we are. There are 1,377 midwives working in DHBs across the country, and that is a record. There are 2,980 more midwives working in our health system. The ministry is aware that there are some urban DHBs that experience difficulty recruiting sufficient midwives, but this is a distribution issue rather than an issue of short supply. The ministry has a number of initiatives to support local midwives and new graduate midwives, through voluntary bonding and locum support. We are also successfully recruiting overseas.
Dr Clark: Does he accept responsibility for the fall since 2013 in the number of midwives per capita employed by DHBs under his watch?
Ms Wagner: I know that the member is new to health, but he may not have heard what I said. There are 1,377 midwives working in DHBs, and a record 2,980 working in our health system. [Interruption]
Dr Clark: Does he think it is acceptable that new mother Lisa Calino, who needed to go to the bathroom and had just had a caesarean, was told by a nurse that she had to move and put her son back in the cot herself, because the nurse on call said: “You’ll have to do that. We are understaffed.”?
Ms Wagner: I am always very sorry to hear that circumstances are such that our healthcare has not met the expectations of all mothers. But I would like to report what the norm is. Our survey says that 85 percent of new mothers report that they are satisfied or very satisfied with their time in labour and birth, and 90 percent of new mothers said that they were confident or very confident in the skills of the care that they are getting in hospital, and 80 percent of them were satisfied or very satisfied with the overall care that they received after the birth. So I am very sorry for your patient, but that is not the norm.
Dr Clark: What outcomes has Health Workforce New Zealand’s midwifery strategic advisory group delivered in light of the comment of the chief executive of the New Zealand College of Midwives, who sits on that group, that “We just meet. That’s all we do. Nothing happens.”?
Ms Wagner: I am very sorry to hear that comment. They tell me that they are working very hard and delivering better health for mothers and babies, and certainly we are resourcing them to do so.
Dr Clark: What responsibility does he take for the significant funding problem that sees the Waikato District Health Board 22 full-time midwives down and Capital and Coast District Health Board nine midwives down, and that sees DHBs like Waikato expected to make savings in nurse vacancies to manage its deficit, and is he confident that all funds allocated to DHBs for maternity services are entirely being spent on maternity services and not being used to fund other overstretched services?
Ms Wagner: Yes. We are sure that they are using their money for maternity services, because we are prioritising the health of mothers and babies. What is more, the member—I know he is new to health—is absolutely wrong when he says that we have had less funding, because we have increased our funding by $4.3 billion. We have moved it from $11.8 billion to $16.1 billion, which is the most money that has ever been spent on health, and certainly we are right behind mothers and their babies.
Green Party health spokesperson Julie Anne Genter:
“It’s shocking just how low levels of pay are for midwives. I have heard on an hourly basis it may be as low as $4 or $5 an hour. That’s outrageous and unacceptable for such an important profession, with such a high degree of responsibility and care. This needs to be changed. We need more, and decently paid, midwives.
Midwives provide fantastic care for new mothers, but they have to cover for a patchy and overstretched health system that isn’t designed for them. Midwives have been consistently undervalued and underestimated in the wrap around care that they provide by a traditionally male dominated health system.
There has been a calculated decision to pay women less than men, to dismiss the work that women do as unimportant, as mere ‘women’s work’. Being a midwife is the epitome of this. We know that guiding women through a birth is quite often life changing work, and it needs to be recognised as such.
We can fix the gender pay imbalance in this country and ensure that every woman is paid what she’s worth, but we need a real commitment from the Government to make it happen.
The National Government will need to financially prepare itself to pay women in the public sector, like midwives, more in Budget2017.
The Green Party are prioritising seeing women like midwives paid more, and will be campaigning on it this election.”
New Zealand First Health Spokesperson Barbara Stewart
New Zealand First also share concerns around the underfunding of the maternity sector. This is reflective of a public health system under immense strain. We know that midwives are facing an unprecedented level of stress as demand for services increase and they are forced to do more with less. This is not a safe environment for mothers and babies.
Midwives undertake such an important role and we want to ensure that they are operating in the safest system possible, therefore, we have been calling on the government to order an independent review into maternity services. Our hope is that changes can be made to help minimise preventable deaths and permanent disabilities.
***
It’s probably best to end again with our midwives. Karen Guilliland, Chief Executive, New Zealand College of Midwives has been speaking out for midwives. Here she responds to our post:
Congratulations and thank you to The Spinoff Parents for giving midwives a voice. It is deeply upsetting to read the concerns of so many midwives about the demands now being place on them. But it is also encouraging that they have been able to speak and hopefully command attention from the decision makers in the health service who have the ability to make a difference to their working conditions. Midwives have been telling the New Zealand College of Midwives, their professional organisation for years that working conditions were deteriorating. And we have been warning the Government and district health boards for years that midwifery was becoming seriously underfunded, mis-managed and ignored. It does not seem to occur to politicians and health managers that to deny support for midwifery is to deny support for New Zealand’s mothers and babies.
It was because our warnings were ignored that the New Zealand College of Midwives, as the professional organisation for midwives decided that it had no choice but to launch a legal action against the Ministry of Health in 2015 to obtain fair pay for our self employed midwives. We alleged discrimination on the basis of sex, midwifery being a mainly female workforce. That action is on hold while we attempt to reach an agreement through mediation.
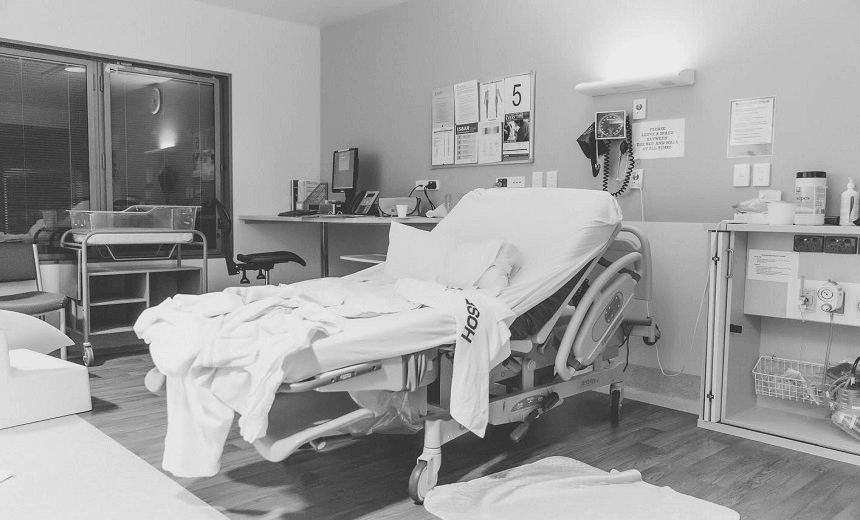
Meanwhile the strains on the ‘core’ midwives who work in hospitals have become headline news because women have begun to complain about the service they are receiving on maternity wards.
But women are not blaming midwives. They have realised that the problem is with the way the midwifery workforce is managed and resourced. The College and the midwives’ union MERAS have been warning district health boards about this issue too but progress has been painfully slow.
Sadly, we now have a crisis in maternity care. We must make the decision-makers listen.
So what can you do to support our midwives? Send comments to The Spinoff Parents and other media, write to your MP, write to Health Minister Jonathan Coleman and share your thoughts and stories on social media. Look out for events to support in your area on 5 May: International Day of the Midwife.
Follow the Spinoff Parents on Facebook and Twitter.
[contact-form-7 id=”249″ title=”Flick Connect Form”]