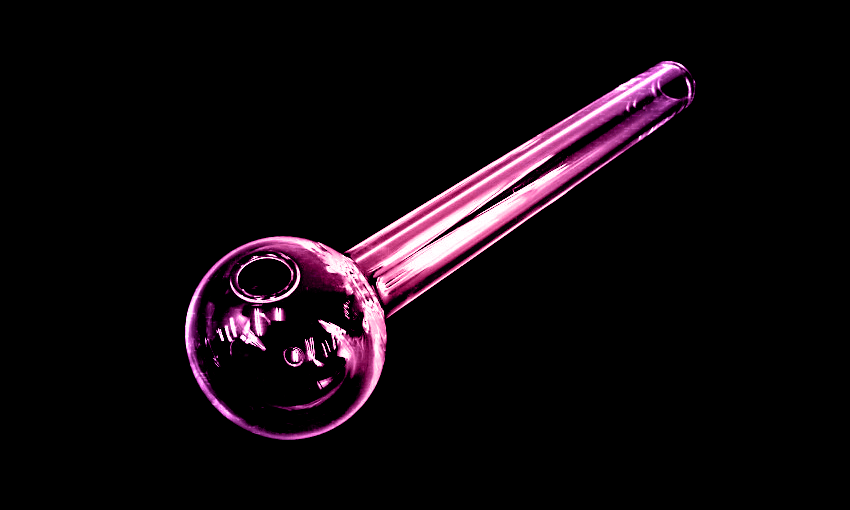
It’s no secret that New Zealand’s methamphetamine use per capita is among the highest in the world. James Borrowdale talks to three people whose lives have been impacted by using meth, about how the drug infiltrated their lives.
Content warning: This feature contains descriptions of sexual assault and drug use, which may be triggering to some readers.
“Immediate euphoria.” Almost all of the various desires of the human body and mind disappeared as the meth flooded Oscar’s* brain with dopamine. The 35-year-old Wellingtonian had tried the drug once before, years ago, but hadn’t been that impressed by the experience. This time, however, “with some high-purity meth”, it was immediately different: “This, this feeling of needing,” he says, “you don’t need anything.” It was all brushed aside by the power of the drug. “Just gone, except for the sexual ones.”
Oscar, also an alcoholic, has a long and varied history with drugs. When he was young, it was psychedelics that most interested him, but as he got older, he says, “much more abusable substances ended up just filling all the gaps in my life”. The meth that gave him his first pleasurable experience with the drug came into his possession when a customer – Oscar was dealing other drugs at the time – offered to clear a debt with the substance. “It’s unfortunate,” he says, “I wish I hadn’t messed with it.”
Meth has slowly come to dominate his life, its “insidious” creep making it hard for Oscar to pinpoint exactly when he lost control. About five years ago, he thinks, was when he “started habitually using without any sort of proper decision-making process that I was actually fully in control of”. It snuck up on him, he says, in much the same way that his drinking did.
When his use was at its heaviest, he was using up to four times a week. Now, having just lost his job as a healthcare worker and “broke as shit”, his usage has come down. He is, he says, better able to keep sight of his priorities – his family and friends, his cat – than some of his meth-using acquaintances have been, and that keeps him from losing everything in pursuit of the drug. “But I don’t feel in control of it, and my attitude and ideas about whether I want to do it or not can just change on a dime. As soon as my situation gets a little bit difficult, or whatever, you know – it’s a fucking hell of a drug.”
It’s also a drug, as the world-renowned Christchurch Health and Development Study found in 2020, that 28 percent of middle-aged New Zealanders have at least tried; 11 percent have used monthly for a period of time, and 4.9 percent have done the same weekly. Another study found New Zealanders were in the top five consumers of methamphetamine globally, with wastewater testing revealing the country consumed 14.1 kilograms of the drug every week between November 2018 and February 2020.
The New Zealand Drug Foundation’s State of the Nation report from 2022 found that “1.2% of NZ adults aged 16+ consumed amphetamines (including speed, Ritalin and methamphetamine) in the past year – around 40,000 people,” not including those using through medical prescriptions. The report found that approximately 9,000 people use amphetamines monthly or more frequently.
It is, behind cannabis and ecstasy, the third most commonly used illicit substance in the country – and one that can find a home in any community.
Jeremy*, 25, grew up in Southland, in what he describes as a “Pākehā, very stable, middle-class family”. “At home, everything was pretty ship-shape, to be honest.” Even so, when he was about 16, he started to use Ritalin, the prescription medication used to treat ADHD, recreationally. His girlfriend at the time was never “super OK” with the Ritalin use – and when the couple went through a bad break up, his act of misplaced revenge against the memory of the relationship was to “start using more and more Ritalin and start using intravenously to get a better high. And yeah, eventually I just kind of jumped up the ladder.”
The family had by now moved to Wānaka. An older acquaintance came over one night and told Jeremy they were going out on the town. “But no, we just went and smoked meth in his car. It was quite confronting. I sort of had the sense that, you know, if I said no things might go badly because this guy was already fried up and wired. It was definitely a confronting experience. But once I smoked enough of it, it definitely reels you in, you know, on that first hit.” It was like, he says, “somehow you’ve been born for the first time, you’re experiencing the world in a whole new light”, even if the two of them did nothing more interesting than “smoking gear on the couch”.
When he later moved to Auckland to study as a 17-year-old, his earlier experiences with the drug – there’d been another occasion, a New Years Eve – meant that when he was asked by one of his classmates whether he used, and feeling in a “not-so-great space”, Jeremy replied, “Yeah, I smoke meth.” His new acquaintance immediately said, “‘Mean, let’s ditch course, we’ll go to my place, we’ll puff up.’ Which is what we did.”
Initially, Jeremy would use meth with his new friend once or twice a week. But three months into what should’ve been his course, “I was at his house every day. I wasn’t studying, I wasn’t going to my classes, and I was just smoking meth 24/7, awake for 10, 12 days at a time.” The thing that jumps out to him most about his descent into full-blown addiction was, like Oscar, its deceptive nature. “For a while you don’t realise that you’re addicted, you think you just really like it.” But then, suddenly, he realised the changes that had occurred in his moral outlook. “You catch yourself fucking robbing somebody or running into a supermarket to steal cheese or wine or honey or whatever. You catch yourself doing things that you would have never normally done.”
One experience, far from normal, lingers in his mind. His friend, unbeknownst to him, had picked up a gram from a dealer with the promise to pay later; together they smoked it. Jeremy was lying on his friend’s couch, trying to sleep. “This weird old man came in, just broke open the front door. And he’s got these two really big dudes with him.” They both had guns, the older guy had a sword; Jeremy thinks he probably had a gun too. “This dealer says, ‘You haven’t paid your tick for the bag I gave you.”
The dealer – “late 50s, early 60s, Pākehā guy, a generally really creepy old man” – then said that the price had just gone up: “It’s not $600 anymore, it’s gonna be $1000.” He was brandishing the sword, telling Jeremy and his friend that “you guys need to get this $1000 bucks together or we’re gonna cut you up”. Jeremy, thankfully, still had his course-related costs – $1000 from Studylink – sitting in his bank account. “Otherwise we might not have gotten out of that situation. I wasn’t allowed to leave; I was collateral. So my friend went out and got $1000 out of the ATM, came back and gave it to the dealer. He ceased trying to sexually assault me. And then just said, ‘Cool, thank you for your business.’ And they all left.”
Aaron*, 30, first began combining drugs – then it was cocaine, MDMA, mephedrone and GHB – with sex when he lived in London. He had previously found it difficult to meet and connect with other gay men, and the drugs had a way of facilitating the intimacy he craved. “Being high… I was confident and it was very easy, you know, to go and meet guys and have sex and perform and speak your mind.” Methamphetamine – the primary ingredient of the chemsex scene – was always around, but in London at least, there was always “another option on the coffee table” and he never felt the need to act against the instincts of a New Zealand upbringing that had demonised meth as an instantly addictive and destructive substance.
When his two-year visa expired, he moved to Melbourne, hoping to extend his time away from Aotearoa. One evening, on Grindr, he met a man who offered him cocaine. Aaron went to his house and accepted a drink. The next memory he has is of waking up in a bed, with his assailant injecting something into his arm. He couldn’t move. “And, yeah, he raped me like several times.”
He moved back to New Zealand, settling in Northland, and started processing the trauma of the rape. He began seeing someone. He moved to Auckland and enrolled in university. London had taught him the pleasures of combining sex with drugs, and Auckland, without steady access to the drugs to which he’d become accustomed, added methamphetamine to the mix. “When I was feeling really down or low, I would jump on dating apps and go and seek chemsex. I was suffering PTSD at the time too. I wasn’t sleeping. I was up at all hours of the night and those are the hours when you want to be looking for that sort of thing.” He’d find himself at someone’s house, early in the morning, smoking meth and then having group sex – “and then drugs and then sex and more drugs, and then a lot of time on Grindr looking for other people to join”.
The days after were always accompanied by “such deep regret”, and he would spend them researching the therapy he needed, the help available. “It was,” he says, “a behaviour I felt I couldn’t control.” He was convinced that he was an addict, destined to end up on the streets. “I felt crazy at the time,” he remembers. It wasn’t until his boyfriend found out about the chemsex, and Aaron decided to try and save that relationship, that he made any real-world steps towards rehabilitation.
He didn’t feel comfortable in the group therapy sessions he initially attended, and it wasn’t until he started seeing a therapist – first funded through ACC, then by his parents – that he was able to begin to truly process his trauma. He was diagnosed with anxiety, depression and PTSD and was disabused of the notion that he was an irredeemable meth addict – just that he engaged in this behaviour when he was feeling certain ways. “Within the first six months there was just like a huge change.” He relapsed just once after he started seeing a therapist, and now has been meth-free for years.
For Jeremy, the experience of being held at gunpoint gave him pause to think. “That was pretty much the moment that was the wake up call that made me think, ‘Right, I want to get out of this.’” He stabilised his use, cutting down to 250 milligrams a week – and stopped seeing that friend. Gone were the 12-day bouts of sleeplessness. It took a further eight or nine months before he was able to stop completely. He calls it “the process that you go through to kind of get yourself to a point where you can stop”. It was a big lesson. “It can be very easy to sort of get a little apocalyptic about the whole situation, because you’re a meth addict now, what the fuck else are you going to do? It is just a process. And if you practise healthy use and maintenance and stuff like that, you can alleviate a lot of the symptoms of being an addict.”
Oscar is yet to find a way out of his meth use, though he dearly wants to. “It bothers me a lot,” he says, and the financial drain of the habit makes him fear for the future. “Pretty much all the goals that I have require me to save money. So if I can’t do that, well, what is there, there’s nothing, is there? I want to knock it on the head. But it’s more than just making the decision; I’ve made the decision dozens of times, but it is a tough one to get rid of, it really is.”
*Names have been changed
If the events depicted in this story have been triggering in any way, please consider contacting any of the following organisations:
Safe to Talk
ACC’s Find Support
HELP
Women’s Refuge
Rape Crisis
Lifeline
For information about how to stay safer if you’re using methamphetamine, and advice on making changes, visit The Level.