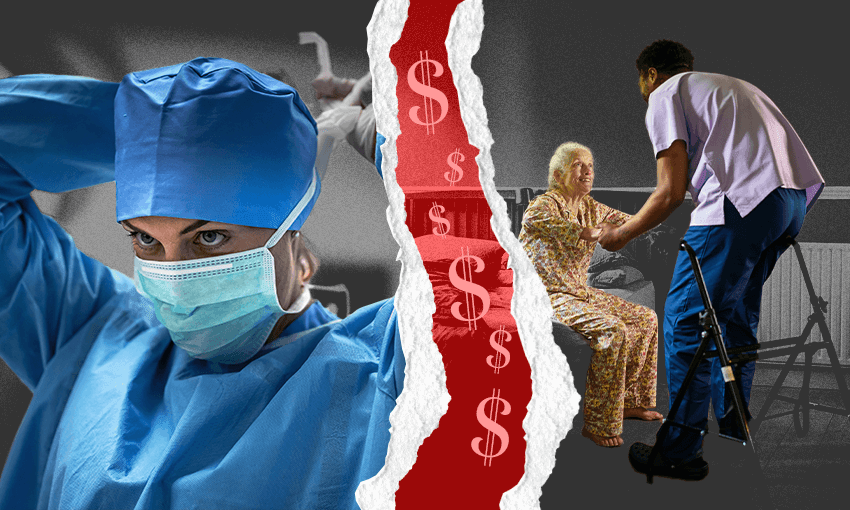
Nurses, teachers, med students, midwives and social workers are among professions that require students to complete unpaid work placements to qualify. A campaign is seeking to change that reality.
“It’s really hard to write an essay when you’ve only had two hours’ sleep because you’ve been up all night attending a birth,” says Ariana, a final year midwifery student. She knows this from several years of intense tiredness, words from lectures mingling with midnight scenes of new life coming into the world. “You feel so helpless.”
Based in Auckland, Ariana started studying midwifery because she loved the idea of being a companion to people giving birth. “I thought to myself: what’s a feminist job? Being a midwife!” Since she started training, Ariana has experienced many “beautiful moments”, but the strain has taken a toll: months of being on call, having to attend at least 40 births and record 2,400 hours of clinical work – more than a year of full-time work – all without pay. “I started off filled with passion and motivation and absolutely loved going to placement… now I don’t know if I want to be a midwife anymore,” she says. As we talk, Ariana is driving home from her current placement; she has moved back to her parents’ house because she couldn’t afford to keep flatting while completing her degree.
To Ariana, it feels like the unpaid work asked of midwives is part of a system that rewards professions that make money rather than make a difference. “Midwifery is the starting point to health for infants, and health for us all,” she says. It almost seems like the rewarding, essential nature of the work is supposed to be compensation enough for its trainees, she says – which seems unfair, given that other types of jobs with mandatory work placements, including police and trade apprentices, compensate trainees financially.
Thousands of people are asking for change
Ariana is one of more than 10,000 signatories to a petition from Paid Placements Aotearoa. The campaign is asking for a stipend for students who are required to participate in work placements as part of their study. “I’m sick of stories about chronic workforce shortages,” says Bex Howells, a campaign spokesperson. “Come on, the solution is right on our doorstep – it’s just about making all professions even.”
It’s not just midwives; teachers, nurses, doctors, social workers and counsellors are all expected to complete work placements as part of study, which are almost completely unpaid (medical students do receive a stipend in their final year, but start placements in their fourth year without pay). Demanding work placements on top of having to attend lectures and do assignments can make it difficult or impossible to have a paid part-time job as well. Student allowances and student loan living costs can be up to $316.39 a week, but many students find this doesn’t cover their costs. “When you’re paying $250 for rent, and you have to pay for parking and petrol and all the other cost of living stuff, it’s a big stress financially,” Ariana says.
Introducing a stipend for students training on-the-job isn’t such a radical idea, Howells points out. Not only do paid training options, including a training wage, already exist in New Zealand, Australia has just introduced a means-tested study support for midwives, nurses, teachers and social workers in its annual budget.
Unpaid work has a major effect on how many people complete their study. Research by Health New Zealand Te Whatu Ora has shown that the financial stress of attending a placement often increases attrition rates, and more than 40% of social workers drop out of training due to financial hardship. Campaign spokesperson Howells says she was first drawn to the issue when trying to study to be a social worker as a mature student, noticing that most of the people training alongside her were also women, often trying to work while parenting or paying a mortgage too. “I couldn’t afford to work for more than three months without pay, I wasn’t going to risk my sanity and safety for it, so I dropped out.” She’s heard similar stories again and again. “It’s tough to put your life on hold and not be better supported, or even know if you’ll come out with a degree at the end,” agrees social work student Tracey Wallace-Hutchins.
“We really need people in these professions, but the norm is financial hardship,” says Hana Pilkinton-Ching, vice president of campaigns at Victoria University’s student association (VUWSA). Students on placement often need hardship grants, or support from association services like a food pantry and advocacy help, she says.
Gender, regional difference and migration status play a role
Howells points out that the nature of the professions that expect trainees to complete placements without pay are often dominated by women – as if the patriarchal expectation that women perform domestic labour for free has been extended to caring professions. “If you want to increase diversity in the workforce, you can’t do it like this, because people can’t afford to work for free,” she says.
Green MP Ricardo Menéndez-March, party spokesperson for social development and employment, agrees gender plays a part. “There is clearly an issue in terms of how gender inequities are experienced – because social workers and nurses are more often women than professions that are paid to train, like police and tradies. It entrenches a gender pay gap,” he says.
Because of the lack of pay, training and study that require unpaid placements often exacerbate other kinds of stress. For example, Rosa is a counselling student, studying alongside a full-time job in the education sector. She moved to New Zealand 10 years ago and has three young children here, while the rest of her family live overseas. “Even though I have a flexible job, it’s a struggle running from one place to another,” she says. To manage her work placements, her kids and partner have had to adjust their schedules. “It’s been a big juggle for everyone; if I was paid I could balance my workload better.” Because her wider family don’t live nearby, she also doesn’t have them as a source of support.
As it is, Rosa has minimal control over her schedule; she’s limited by the number of clients and hours that her workplace gives her. Allowing students more preference about where they get placed is one of the elements of Health NZ’s placements research. Rosa would like to see more clarity around expectations for students with mandatory placements, as well as payment for mandatory work training.
Students on placement also face other barriers, like travel costs. Wallace-Hutchins is doing a social work and health science masters concurrently; she lives in Te Puke and studies by distance. As a disabled person and non-driver, getting to her placements has been a struggle. “Organising a placement locally that would accept me, then figuring out how to get to the workspace was huge; I can’t just jump on a bus, because we don’t all live in cities.” For her, any support for students on placements has to take into account the needs of people in regional areas. “We need to strengthen the social work workforce, especially in the regions,” she says.
Opposition politicians support change
After the announcement from Australia, opposition politicians expressed interest in seeing a similar policy in New Zealand. “We’d like to see a more universal approach [rather than means-tested] – paying people for placements is a long-term investment to see more people finishing their degrees,” says Menéndez-March. He has first-hand experience of the struggle of unpaid placements: before becoming an MP, he was a field education coordinator for social workers with placements at community group Auckland Action Against Poverty. “It was hard as a field educator knowing that if I made students do their full 40 hours, I would compromise their ability to pay rent,” he says – as working a 40-hour week left no time for them to do paid work.
Menéndez-March points out that for occupations like nursing, which require hours of work placements, the only realistic path for addressing the severe workforce shortage currently is immigration. “Paid placements would make it easier to domestically recruit for these roles,” he said. “With many job losses currently, and many people needing to retrain, this is a timely moment to look at this issue.”
Carmel Sepuloni, Labour spokesperson for social development and employment, said that while in government, her party looked into the issue of paying people for their placements. “Ministers … discuss[ed] how we could better support people taking up training in these areas with highly feminised workforces and workforce shortages,” she said in a statement. While Labour has no specific policy around placements currently, she said she was keen to hear from people about the issue.
With regards to health workforce training in particular, Health NZ’s director of workforce planning and development, John Snook, said that decisions about pay and mandatory hours were up to individual institutions of study and registration bodies. More than 21,000 students in health professions take part in clinical placements a year, amounting to more than 290,000 weeks of practical learning requiring coordination and supervision across hundreds of locations. The new digital system for coordinating placements will be implemented from later this year, said Snook.
To Howells, who is now doing her master’s research on student work placements, the inequity created by paying only some students to train on the job is stark, and has a profound impact on thousands of people. But beyond those in training, she said the issue affects us all. “If you’ve ever waited weeks to see a doctor, months for mental health support, seen how overworked your kids’ teachers are, or struggled to find a midwife for your maternity care – you’ve come into contact with this issue. The long-term goal is accessible services for all communities and for people to be paid to train in these roles that really matter.”
Rosa and Ariana’s names have been changed.
Comment for this story was requested from the minister for social development and employment, Louise Upston, but this was not provided in time for deadline.
This article has been updated to reflect Health NZ’s request that student clinical placements be characterised as learning, rather than work.