Nine weeks on, the Auckland outbreak has hit record levels, and continues to grow. The numbers tell a compelling story, writes Siouxsie Wiles. Data visualisations by Harkanwal Singh.
The Spinoff’s ongoing coverage of Covid-19 relies on support from readers via Spinoff Members. Help us stay on the story by joining here.
This week, Aotearoa recorded its highest daily number of confirmed Covid-19 cases since the pandemic began. That number – 94 – is still minuscule by international standards, but don’t let that fool you into a false sense of security. Let’s look at the data and see what we can learn from it.
We’re experiencing our biggest outbreak of the pandemic and it’s growing
Looking at the data of when we’ve had community cases in New Zealand, we can see that for much of the pandemic our alert level restrictions and border controls have done a great job of eliminating Covid-19. Until August this year, there had been just over 2,800 confirmed cases and 26 deaths.
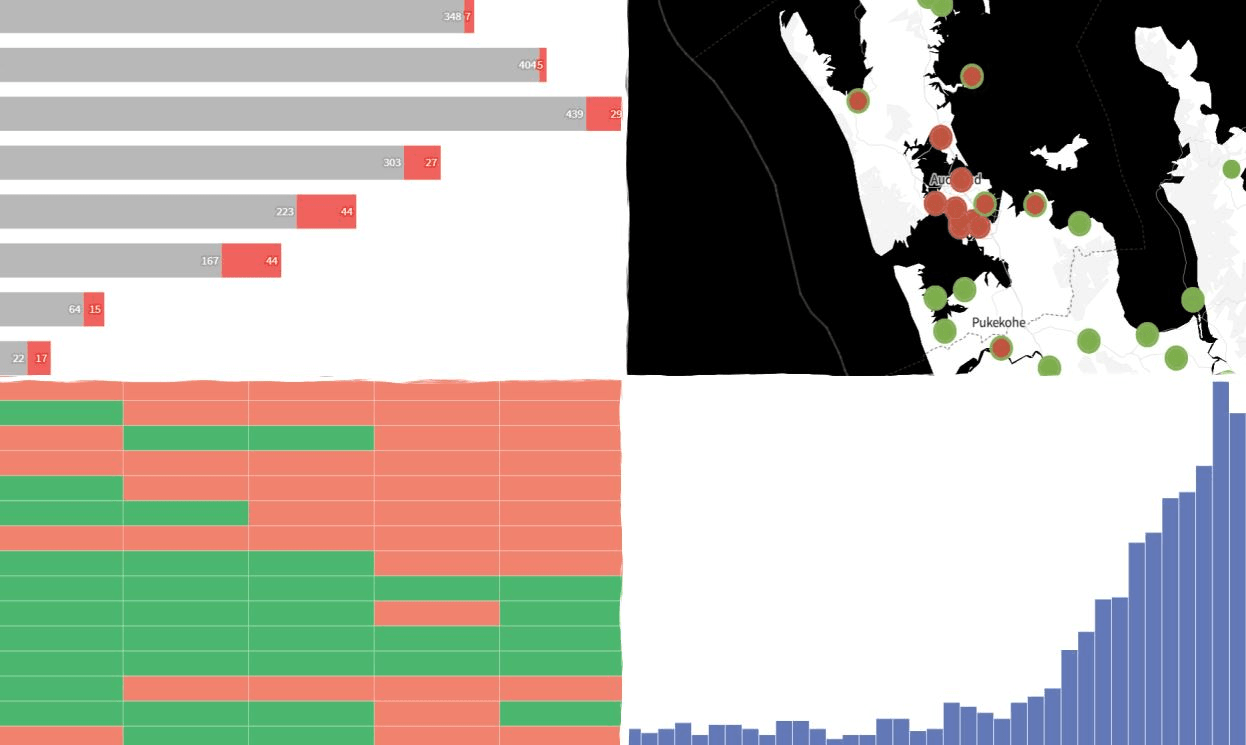
But since delta breached our defences in August, we’ve had more than 2,100 community cases of Covid-19, and two more deaths. Looking at the graph, we can see that the move to alert level four did a really good job of containing delta, but it didn’t eliminate it. It looks like we got close. The sad thing is we’ll never know if staying at level four for a couple more weeks would have done the job or whether the virus had already infected people who either can’t or won’t abide by the alert level restrictions.
Throughout the world we’ve seen what happens when Covid-19 and inequality collide. Now we are experiencing it for ourselves. It’s clear that our response to date hasn’t focused on addressing what makes some people and communities more vulnerable to Covid-19. We’ve seen this in our vaccine rollout, in the way the wage subsidy is paid directly to employers instead of employees, in the lack of any significant increase in benefits, and in the focus on “shovel ready” recovery projects that have tended to provide jobs for men, despite more women being made unemployed because of the pandemic. On top of that, it’s likely this delta outbreak would also have played out quite differently if we had detected it earlier.
Throughout this pandemic, we’ve relied on people going and getting tested if they have any symptoms as the main way of detecting community transmission of Covid-19. Complacency was our enemy here. For the last few years, I’ve been participating in the FluTracking survey. Each Monday morning, I get an email asking me about any symptoms I’ve had over the previous week. Yesterday participants got an email telling us some of the findings from the data for this year. This is the statistic that really stood out to me: on average per week, less than a third of participants with fever and cough reported being tested for Covid-19.
There will be lots of reason for this but what is clear from the early cases identified at the start of this delta outbreak, there have been people with symptoms who thought that because there was no virus in the community in New Zealand they didn’t need to get tested. Unfortunately, they were wrong.
The last thing the graph shows us is that the current outbreak is growing. It’s growing slowly, but it is growing. The reason the growth is slow is because we have restrictions in place. How much cases continue to grow, how fast, and how Covid-19 will impact on our healthcare system depends entirely on when and how we lift the current restrictions and what level of vaccinations we’ve reached when we do. I’ll say it now, but if we opt for some kind of “Freedom Day” regardless of reaching a really really high vaccination rate across the country and across different ethnicities, it’ll be carnage.
Cases are spread throughout Auckland
I think many people were probably shocked when we were told that Covid-19 cases have been confirmed in more than 120 suburbs across Auckland. But the wastewater data has been telling us a similar story. ESR are sampling wastewater from 22 sites across the Auckland region and testing it for fragments of the Covid-19 virus. They put their findings up online on a weekly basis. The data is really clear; detections of the virus have been increasing. If we just look at the last four weeks, we’ve gone from eight of those 22 sites testing positive for the virus to 14. And from the map you can see just how wide an area these positive sites cover.
That means regardless of where you live in Auckland, you may end up being exposed to Covid-19. So please, wear a mask while you are out and about, stick to the alert level three rules, and if you aren’t already vaccinated, get vaccinated. Remember, you aren’t fully vaccinated until two weeks after your second dose.
The ability to detect chains of transmission is buckling under the pressure
Stopping transmission of the virus relies on two important things. The first is identifying where a case got infected and then following the leads from there to identify any unknown cases and transmission chains. This is known as case investigation. Here in New Zealand, that case investigation has been helped by using genomic sequencing which can help link cases together by how related the sequences of the virus are to each other. The second thing that helps stop transmission is identifying people the case was in contact with during the time they were infectious and getting those people into isolation. This is what we know as contact tracing.
For most of this outbreak, Ministry of Health has been reporting the number of cases from the last 14 days that have not been linked to known cases. These are sometimes called “mystery cases”. During September these hovered at between five and 15 per day, as case investigations and genomic sequencing was able to link the cases to each other.
But since early October the number of unlinked cases has been steadily rising and that number is now approaching 200. Because delta moves so much faster and infects so many more people, the outbreak has put huge pressure on our public health units who do the contact tracing and case investigations. The focus has had to shift to stopping further transmission rather than investigating where cases came from. This just makes it all the more important that wherever you live, if you have any symptoms that could be Covid-19, please get tested.
People of all ages are getting Covid-19 and some are ending up in hospital
The delta outbreak is affecting people of every age, with more than 1,200 people under the age of 30 having been infected. More than 40 of them have been hospitalised. In total, more than 170 people have been hospitalised during this outbreak. As cases grow, that number is going to grow, too. And it’s not as simple as prepping more ICU beds. Decades of under-funding means there is no slack in the system. So at some point soon, Covid-19 is going to have a massive impact on the ability of our healthcare system to provide care for non-Covid-related things.
Vaccines are protecting people from severe illness
The good news is that vaccines really are keeping people out of hospital. The majority of people who have been hospitalised have not been vaccinated. And while one dose offers some protection, it’s the people who are fully vaccinated that are most protected. As I said earlier, don’t forget you aren’t fully protected until two weeks after your second dose.
We need to keep vaccinating!
To protect people from getting Covid-19, and to protect our hospitals from being overwhelmed, we need everyone to get vaccinated. Seriously. We need double doses to be up at over 95%. The data shows we’ve still got a way to go, especially in the under 30s.
Even if you are young and healthy, we all need you to get vaccinated. Our under 12s who can’t get vaccinated need you to. As does everyone with cancer, or who is on dialysis. And everyone who is immunocompromised for whatever reason.
As Toby Morris and I have explained before, beating Covid-19 is a multi-player game and we all have our part to play. If you are still nervous about getting vaccinated, or know someone who is, hopefully this FAQ we put together can help.