Despite it being proven that women with dense breasts have an increased risk of developing breast cancer, there is currently no requirement for Breastscreen Aotearoa to inform women of their own density after a mammogram. Shoshana Maasland talks to the women advocating for that to change.
This story first appeared on Te Waha Nui
Fay Sowerby was already involved in breast cancer research when she was diagnosed with the illness. The secretary of Breast Cancer Aotearoa Coalition was well-informed and had been having annual mammograms and occasional ultrasounds. She had recently received an all-clear letter advising she wouldn’t need another mammogram for two years.
Four months later, though, she felt a lump.
“I was in a [store] changing room at Lululemon and I put my hand on the side of my breast and felt a small lump. I had no doubt when I touched it what it was.”
Sowerby immediately booked a doctor’s appointment. By the time she got there, she had found two more lumps. An ultrasound picked up what looked like about six tumours, and three then showed up clearly on an MRI.
The cancer had become invasive. “It was in the lymph node by that time, which is not what you want.”
The mammograms – both the one taken four months earlier and another one taken after she found the lumps – were not clear enough to reveal the tumours, which Sowerby says may have been there for some time.
“You cannot see them, it’s just a white vision. It’s very hard with breasts like mine to detect a tumour.”
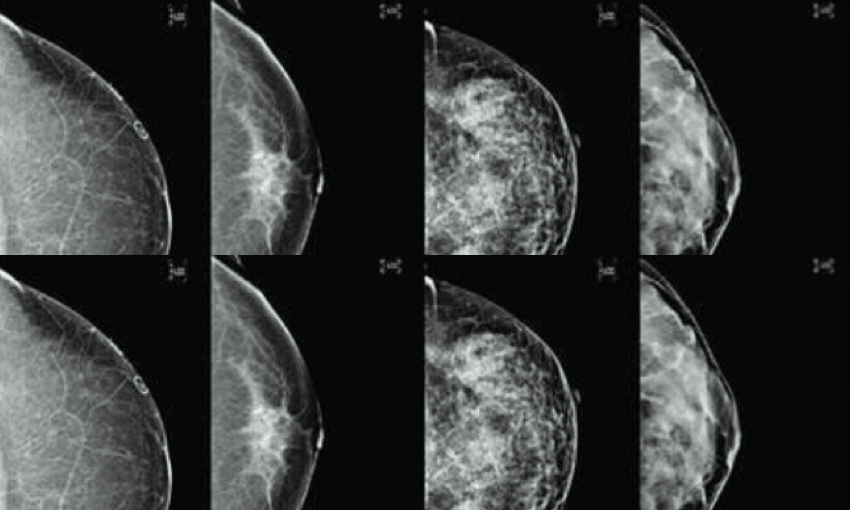
For women, like Sowerby, who have dense breasts – where there is a higher proportion of fibrous, supportive, tissue compared with fatty tissue – that density may mask cancers. Both dense tissue and cancer cells show up white on a mammogram, making it harder to interpret for the radiographer.
And women in the New Zealand public screening system are unlikely to be told if this increased risk applies to them.
Density itself a risk factor
Aside from the masking effect, breast density has itself been found to be a key risk factor for breast cancer. A 2017 US study of more than 200,000 women found breast density was the most common leading breast cancer risk factor.
New Zealand has the 10th highest breast cancer rate, according to the World Cancer Research Fund. The Breast Cancer Foundation reports that New Zealand women have an 11 to 12% risk of developing breast cancer within their lifetime. For women with dense breasts that goes up to 15 to 20%.
In the US, about 40% of women have dense breasts. In New Zealand there is no such data because the national screening service, Breastscreen Aotearoa, does not collect data about breast density, although that information is available to a radiologist in the results of a mammogram.
Women who pay for private mammograms might be informed if they have high breast density, but not women in the public screening system. This is something Sowerby and the BCAC are working to change. “I feel very strongly, as does BCAC, that women have the right to be informed and that information should not be withheld from them. They have the right to the same information that their specialist has access to.”
The Breast Cancer Foundation is also in favour of informing women about breast density. Its research and communications manager, Adele Gautier, argues a mammogram report back to a GP should note the level of breast density. “If you have your mammogram in private, there’s a good chance they will tell you how dense your breasts are, which gives you a heads-up that if your breasts are dense, that your mammogram will be a bit less effective,” she says.
Currently, 38 states in the US require that women are notified about their breast density and there is a federal bill open for consultation which could lead to mandatory notification in all states. The Canadian province of British Columbia followed suit in 2018. In Western Australia, notification of breast density has been mandatory for more than a decade.
Women advocates brought change
Internationally, laws requiring that women are notified of their breast density came about due to advocacy efforts of women such as the late Dr Nancy Capello in the USA, who was diagnosed with advanced breast cancer just weeks after a normal mammogram. In Australia, breast cancer researchers with expertise in mammographic density formed the Information Forum on Mammographic Density Alliance (InforMD) in 2016.
The alliance is working to raise awareness of breast density and has called for national guidelines to be developed urgently so women with high breast density can be notified.
The public debate has reached New Zealand, in large part due to the advocacy of Dr Monica Saini, a US-trained breast radiologist who is currently chief medical officer at Volpara Health Technologies, a New Zealand med-tech company using artificial intelligence to assess breast density.
Dr Saini made public calls to inform women about breast density on Radio New Zealand (RNZ) and through a Ted X talk, in June and August this year, respectively. The Ministry of Health has clearly been listening; papers obtained from the ministry under the Official Information Act (OIA) revealed that increased public attention from Dr Saini’s appearances was a factor in the prioritisation of a review of the information provided to health professionals on breast density and the proposed production of a pamphlet for screening participants.
The papers also show that the first minuted discussion of breast density took place the same day that Dr Saini raised the subject on RNZ. Since that interview, the papers reveal that “three women mentioned breast density at their appointments and subsequently [Breastscreen Aotearoa] have received a complaint that will likely go to [the Health and Disability Commissioner].”
Although growing public awareness is clearly on the ministry’s radar, it does not appear to be looking to change its policy. Its new Breast Density Information Sheet for health professionals, posted on its website in September this year, acknowledged that “increased breast density is a known risk factor for breast cancer”, but said that, since mammography became digitised, the masking effect of dense breast tissue has become less of a risk.
It said that there was insufficient evidence to recommend additional testing, such as ultrasound or MRI, and that “the harms of extra imaging, such as causing anxiety, unnecessary needle biopsies, over-diagnosis and cost, are likely to outweigh the benefits”.
It appears New Zealand is following Australia (not including Western Australia) and the UK, which have decided not to assess, or record breast density or provide supplemental testing until there is established best practice for how it should all be provided.
The Royal Australian and New Zealand College of Radiologists put out a position statement in 2016 recommending against reporting breast density to women for similar reasons to those provided by the Health Ministry. Despite the public interest and commentary on the subject, they say that their position has not changed since.
A complex issue of priorities
If there is any consensus around this issue, it’s that it is far from black and white. While the science is clear that breast density has an impact on a woman’s breast cancer risk, there is debate about what effect notifying women and doing further screening would have on breast cancer survival rates.
Then there is the resource issue; even advocates for notification and/or further screening, such as Dr Saini, recognise the difficulties for the Ministry of Health in accommodating all the extra screening in an already overstretched and under-resourced system. “We are definitely under strain. Right now, the number of breast radiologists we have to interpret mammograms is in a dire shortage, and probably in the next five years, when a number of people come up to retirement age, we’re going to be even more strained than we already are,” she says. To add to the pressure, the government has recently pledged to extend the screening age to 74.
Among those with misgivings about the value of notifying women about high breast density is Dr Rob McNeill, a senior lecturer in health systems at the University of Auckland, and a specialist in cancer services and cancer care.
“There’s no doubt that for some women, knowing that they have particularly dense breast tissue is going to mean that they’re going to be a bit more observant, talk with their health professionals a bit more about doing extra screening and extra tests, and that that may help them get diagnosed earlier.
“And it may end up that that earlier diagnosis leads to a better outcome for them, but I think it’s really unclear at the moment how much harm the extra testing would do.”
That harm includes “complications from the biopsy procedure, anxiety and stress around being told that there’s something that needs to be investigated, the stress and worry that goes with going through treatment, and the harm from treatment, [and] the sorts of surgery and/or chemotherapy that are involved with the treatment of tumours that wouldn’t otherwise cause these women any harm”.
Additional screening, in particular ultrasound, could “throw up a lot more false positives, and it would then lead to a lot more women needing needle biopsies, and potentially being diagnosed with tumours that are potentially not harmful to them, but they would then have treatment for them and be harmed by the treatment,” he says.
A small proportion of these women would be harmed by the diagnostic procedures, Dr McNeill argues, and a larger proportion (although still a small number) would be harmed by the treatment, when the tumours themselves might never have actually caused harm, such as would be the case with ductal cell carcinoma in situ (DCIS).
This is a type of tumour that, for many women will never go on to spread if left alone, he says.
Ask a woman
Dr Saini concedes additional screening may result in more false positives. “It is a big deal to put women through the anxiety of a false positive.”
However, she pushes back on the argument that further testing might pick up tumours that wouldn’t cause problems. “I don’t buy that. There is a spectrum. Some of those small DCIS cancers can sit around for 10 to 20 years. What we don’t understand about those cancers is what triggers them to switch into fast growing DCIS and eventually into invasive cancers.
“So treating those cancers is absolutely vital. If it’s a fast-growing cancer you might be able to catch it if it’s a small enough size, and the cure rate of cancers under 15mm is extremely high.”
Another argument against notification that Dr Saini has little time for is the one claiming that it would cause unnecessary anxiety. “I would say, ask a woman.” She points to a study from Western Australia, where women have been informed about their density for more than a decade, which showed that while knowing their breast density made some women feel anxious, it did not deter the vast majority of them from attending screening.
“If you ask all these women who’ve had cancer and gone through the treatment, all of them say, ‘Yeah, I might be anxious about it but I’d rather know and make a decision as to what I’m going to do’.”
Adele Gautier also rejects the “anxiety” argument. “My personal response is, we’re grown-ups. We can be told that something needs to be investigated without losing the plot. I think it’s how you talk about it and how you educate people. It’s an investigation, a process and in most cases it doesn’t result in a diagnosis of breast cancer.
“I don’t think that worrying about people’s anxiety is a reason not to investigate something that you know is a risk factor.”
Both Gaultier and Dr Saini question whether the same issue would be raised in the case of men’s health. Gaultier says: “Do they ever talk about anxious men? It’s very patronising.”
Dr Saini clearly sees this as a feminist issue, putting it in the context of historic medical and scientific bias against women, and outdated ideas about women’s supposed fragility, touching on the Victorian notion of “female hysteria” – the idea that the uterus is the source of a distinctly female anxiety. However, she thinks this attitude is slowly changing. “I think we’re much more aware in this day and age because our access to information is greater, so we can start calling out biases.”
She says progress on breast density awareness has been made because of action taken by women who were personally affected by the lack of information. “The real breast density movement is not because of progressive physicians or researchers who stumbled upon great research.
“The only reason in my opinion that has happened is because of the patients and the women who suffered through breast cancer and didn’t realise there was information missing in the testing they were having, and that information was never conveyed to them, and thus they weren’t able to make a decision because they were never told.
“It’s because of them advocating that this whole field has changed. It’s the patient advocates, the breast cancer survivors, not because of the medical establishment.”
Right to know
Advocates in New Zealand are clear that women should be informed about a matter that relates to their health and risk profile. “I think in this day and age we cannot practise medical paternalism,” says Dr Saini.
But given all the challenges, how might this actually happen? As well as the resourcing issue, there is currently no standard measure of breast density, no plan for disseminating the information, nor the resources to accommodate the additional screening that would result. Gautier argues that for years, radiologists in other countries have been making a visual assessment on density. “It’s not perfect but we feel that it’s acceptable here until they’re willing to invest in the technology that will actually measure it more stringently.
“We know it’s a big challenge for the screening system but it’s one they have to acknowledge and step up and have a plan for.”
In Dr Saini’s view, the way forward is to “keep everyone in the conversation”, be transparent and conduct research. “It’s ok for us as a medical establishment to say, ‘We don’t know’ when it comes to breast density in New Zealand. We don’t know how many women have dense breasts.
“So I think we should be transparent about what we don’t know and talk about how are we going to look at this data from around the world that’s extremely compelling. How do we figure out how it translates here? The only way to do that is to do the research – you’ve got to study the problem.”
Once the issue can be quantified, Dr Saini suggests, it might inform a different screening strategy which perhaps differentiates between different risk profiles, which could prove to be more cost effective.
Fay Sowerby and the BCAC also favour a risk assessment process. There are several tools being trialled internationally that look at the various risks, including breast density, combined, rather than in isolation. “It’s moving from a population base to segmenting and stratifying women in terms of who needs more screening and who needs less screening. And individual choice needs to come into it as well,” says Sowerby.
There’s no evidence that there is appetite from the Ministry of Health to look further into this question in the near future. The government announced the New Zealand Cancer Action Plan 2019-2029 in August, but it did not mention breast density.
Not our data
On this issue, the government seems content to follow Australia and UK for now. But Dr Saini warns against assuming that data collected from the UK or Australia will be helpful to New Zealand.
“Where’s Māori, where’s Pasifika? Where are the different ethnic populations that make up New Zealand, which is very different from the UK? I don’t think just following them and their guidelines is really the best practice for New Zealand.”
Indeed, meeting minutes obtained from the ministry under the OIA noted anecdotal evidence existed of higher breast density among Māori and Pasifika women.
Considering that “equitable cancer outcomes”, and improving statistics – such as the fact that Māori are twice as likely as non-Māori to die from cancer – are key objectives of the New Zealand Cancer Action Plan 2019-2029, there may be an increase in pressure on the ministry to conduct New Zealand-specific research into breast density, and to ultimately develop a screening plan that takes breast density into account as a risk factor.
Fay Sowerby, who has been advocating for change on this issue ever since her own diagnosis in 2013, knows not to expect rapid change in the public system. “I have learned patience through this process. You need patience in bringing about change in the health system and I understand that.”
Her own experience spurred a desire to help save other women from going through what she went through because it seems unnecessary. “However, I know that every day women continue to go through the same thing.”