The Southern DHB has apologised and pledged to change practices after a report into a young woman’s complaint about treatment which included being stripped naked and left unattended in seclusion for 12 hours. Here she tells her story.
Content warning: this article contains mention of suicide.
I’d forgotten the Health and Disability Commission was about to publish its report. I didn’t realise it was online until someone sent me a message on Twitter on its release last week, asking if it was me. The complaint, which I’d made in 2017, was about a time I was secluded while mentally unwell. I was 18.
My dad called (he rarely calls during the day). He said it was being reported on in the news. He wanted to send an email to Stuff, explaining his anger at the mental health system. I told him to think on it before deciding. I’m angry, too. I read some of the comments on the NZ Herald Facebook post for their article. Many were empathetic, but there were some along the lines of “two sides to every story”. It’s true, there are. I want people to hear mine.
Shortly after turning 18, I was admitted to hospital following a suicide attempt. For the following year, I endured severe, treatment-resistant depression. Around nine months later, I had seven treatments of electroconvulsive therapy (ECT) involuntarily. A lot of people would assume that having electroshock therapy against your will would be the worst thing you could experience in the mental health system. And it did terrify me. But it wasn’t the worst.
In late 2013, I was transferred to a private psychiatric clinic in Dunedin. Mentally, I wasn’t doing well. The incident that has been reported on was one of four times I was transferred to the public locked unit.
I found it interesting that the report said I was in a suicidal state, because that’s not how I saw it. I was a danger to myself, but not for that reason. After refusing medication, I was very sleep deprived, and felt on top of the world. The “verbal disagreement” with another patient involved her objecting to a joke I made, and my indignantly writing out a Stephen Fry quote about people who take offence, and plastering it on the notice board. I left the clinic, under the knowledge that I was bulletproof and could jump off a tall building and not die. I guess I can see how someone might conflate this with being suicidal.
After the police took me to the hospital, I was pinned down and had all of my clothing, including my underwear, forcibly removed. They pushed me to the floor, and hurried out of the room. In the report, the SDHB asserts that I was highly aggressive. I resisted restraint, although do not believe this can be labelled “highly aggressive”. Was such force really required for a not-particularly-strong, five-foot-four teenage girl?
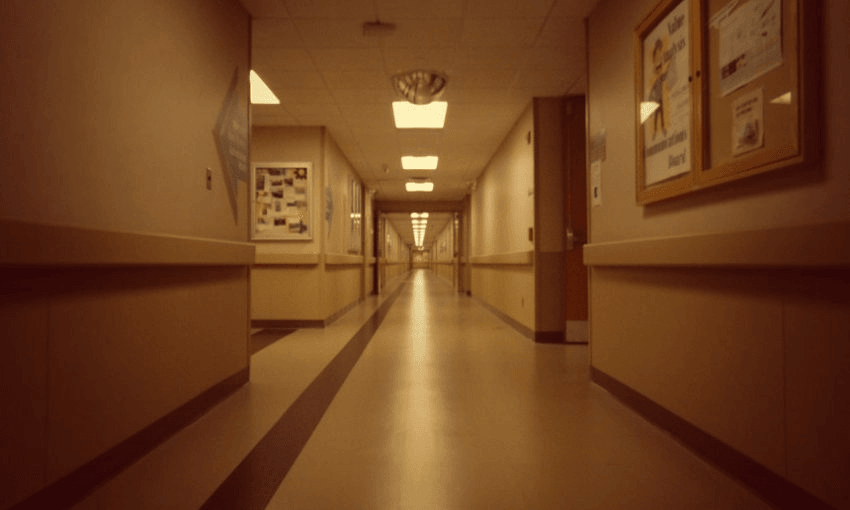
The room was bare, save a cardboard bedpan and a tear-resistant blanket. No mattress, no pillow. I didn’t use the bedpan as a toilet; I pissed on the floor. There was even a plughole, which I assume meant I wasn’t the first person to do so. It wasn’t (just) a rebellious act – I wanted to use the bedpan to rest my head on. It was cold on the hospital grade linoleum surface. I didn’t feel on top of the world any more. I felt powerless.
The experience was humiliating. But it wasn’t the only unacceptable thing to happen while in hospital. It was just the only incident I made a complaint about. In Wellington, I was attacked by a female patient with gang associations. They separated her from others in the ward for only an hour or two. When they brought her out of the “de-escalation area”, she threatened me on the way back to her room, which was near mine.
The next day she attacked another patient, and the police were involved. Funnily enough, we ended up being friends. The nurse who was there when she assaulted me said it was categorically not my fault. Another nurse, who wasn’t there when it happened, later told me I had provoked it.
I got an apology letter from the Southern District Health Board recently, at the conclusion of a complaints process, which spanned more than two years. It took me a long time to find it last week – which may be indicative of how much I valued their response. It wasn’t exactly a “sorry-not-sorry” letter as these things too often are, so I suppose it could’ve been worse. The part that stood out to me was, “this has served to remind staff of the standards of care expected of them.” It concerns me that it took a complaint, years after the incident, to remind staff that it was something they shouldn’t do.
It speaks to a certain culture within the mental health system, especially in a hospital setting. There seems to be a lack of accountability between staff members, particularly when it comes to the higher-ups. I want to make it clear that there are a lot of great mental health professionals, too. I currently live in Dunedin, and the community mental health services here are excellent. But in hospitals, where there is such a high level of acuity, and a lot of leeway in terms of what staff can do, people need to be willing to call each other out. Patients are often not in a position to hold staff accountable, and even if they are, there is a huge power imbalance.
I really do hope that my complaint has “highlighted shortcomings” as my apology letter claims. I am not overly optimistic, however. I guess we will wait and see. In making the complaint, I think I gave my reason as not wanting anyone else to experience what I did. And that was definitely a part of it. But it was also about empowering myself, and getting them to admit that I was telling the truth; that what they did was wrong. That’s one of the reasons I wanted to write this piece myself, too, rather than giving an interview. I wanted people to hear my side of what happened, not as part of someone else’s commentary or within medical notes in a report, but directly from me.
Where to get help
Need to talk? Free call or text 1737 any time for support from a trained counsellor.
Lifeline – 0800 543 354 or 09 5222 999 within Auckland.
Samaritans – 0800 726 666.
Suicide Crisis Helpline – 0508 828 865 (0508 TAUTOKO). Open 24/7
Depression Helpline – 0800 111 757 or free text 4202. This service is staffed 24/7 by trained counsellors
Samaritans – 0800 726 666
Healthline – 0800 611 116
Counselling for children and young people
Youthline – 0800 376 633, free text 234 or email talk@youthline.co.nz or online chat. Open 24/7.
thelowdown.co.nz – or email team@thelowdown.co.nz or free text 5626
What’s Up – 0800 942 8787 (for 5–18 year olds). Phone counselling is available Monday to Friday, midday–11pm and weekends, 3pm–11pm. Online chat is available 7pm–10pm daily.
Kidsline – 0800 54 37 54 (0800 kidsline) for young people up to 18 years of age. Open 24/7.
For more information about support and services available to you, contact the Mental Health Foundation’s free Resource and Information Service on 09 623 4812 during office hours or email info@mentalhealth.org.nz