At least three new, more contagious Covid variants have been spreading around the world. Here’s how they emerge and why.
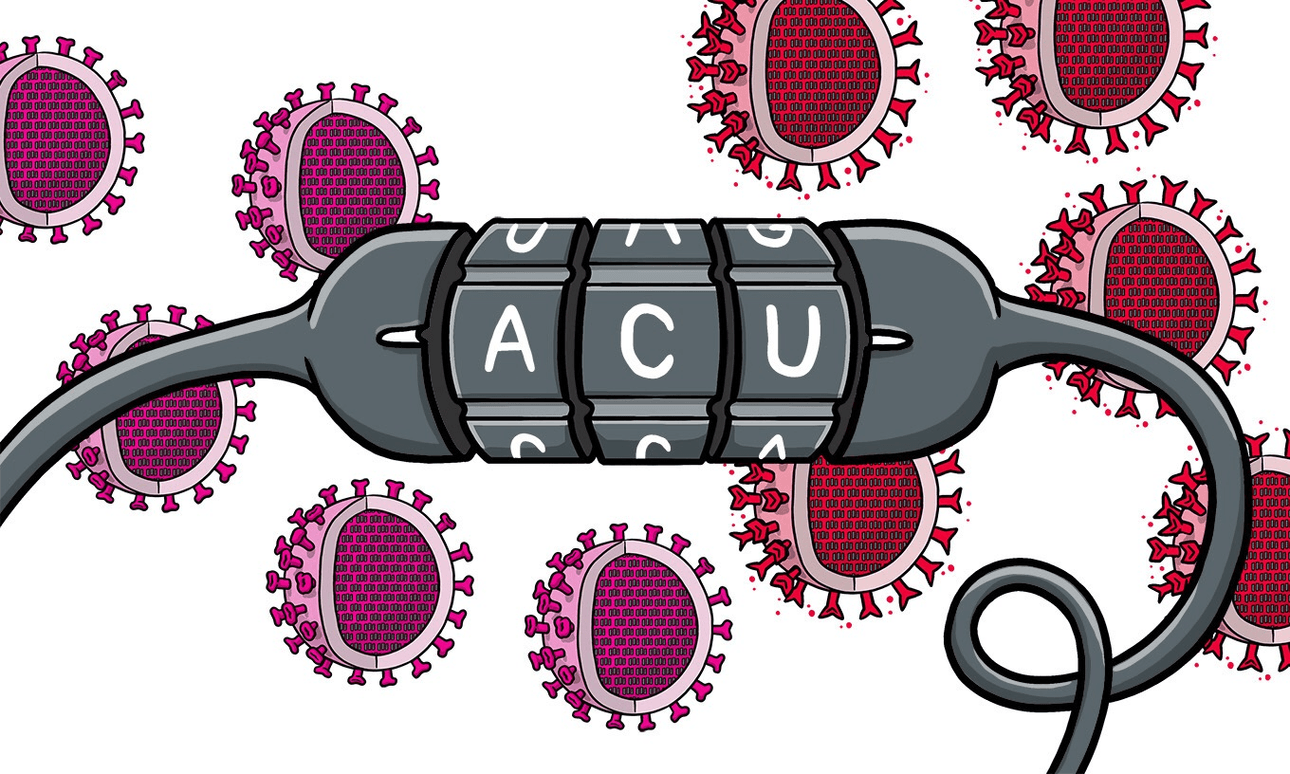
Let’s start with the basics. The genetic material of the SARS-CoV-2 virus responsible for Covid-19 is a strand of RNA made up of almost 30,000 nucleotides. Those nucleotides – adenine, cytosine, guanine, and uracil – are more commonly known by their abbreviations: A, C, G, and U. Nucleotides code for amino acids which in turn give us the proteins that make up the virus, like the spike protein the virus uses to enter its hosts cells.
Each time the virus enters a new host, it turns some of that host’s cells into virus-producing factories. Those cells copy the virus’s genetic material which then gets repackaged into new virus particles. These new virus particles then leave the host and head off to find a new host to start the process again.
Mutations: a chance mistake
When the virus’s genetic material is copied, the wrong nucleotides can get put in place, completely by chance. An A can become a C, say, or a G can become an A. These are called mutations. Genomic sequencing is the technique that allows us to see just how the virus mutates as it moves from host to host. The first SARS-CoV-2 genome, now referred to as the reference genome, was uploaded to the global flu-tracking database GISAID on January 12, 2020. It came from a swab taken from a man in Wuhan in December 2019. Sequencing of more virus samples taken from patients that January showed that some no longer had a G at position 11,083. At some point between December and January, that G had changed to a U. We call this mutated virus a variant – the virus that emerged from the host is a little different to the one that started the infection.
As time has passed, more and more nucleotides have changed. It’s been happening at a rate of about two changes a month. As people have transmitted the virus around the world, different changes have been accumulating in the virus in different parts of the world. This has given rise to what we call lineages of the virus. It’s a bit like looking at a family tree. Using genomic sequencing, we can see how the different lineages have emerged and how they are continuing to change.
Beyond lineages: what difference do mutations actually make?
OK, so here’s the important bit. Mutations can have no effect on the virus at all. Or they can change the amino acid that’s coded for by the nucleotide at that spot in the virus’s genome. Depending what the amino acid changes to and where it is in the protein it makes, a mutation can have no effect on the virus, or it can give it an advantage or even a disadvantage when it comes to infecting a new host. Also, depending on what the protein does, mutations can change how the disease plays out for the infected host.
A virus that has a disadvantage will tend to die out. In other words, some mutations are basically dead ends for the virus. But what about the mutations, or combinations of mutations, that give the virus an advantage, like making them more infectious or helping them evade the host’s immune system? Variants with these can end up becoming dominant as they outcompete all the other virus variants that are around at the time.
Variants of concern and why we’re hearing so much about them right now
In terms of the pandemic, the theme for January 2021 has been the emergence of what are sometimes being called “variants of concern”. First it was B1.1.7 (also referred to as 501Y.V1, or VUI-202012/01) which emerged in the UK, then B.1.351 (501Y.V2) identified in South Africa – the variant that has been contracted by the Northland woman – and more recently P1 in Brazil.
The important thing to understand though, is that it’s not really the variants themselves that are of concern, but the set of mutations they each have. Sets of mutations that can give a particular variant of the virus an advantage. From lab experiments, we are starting to understand which mutations, or combinations, can improve the ability of the spike protein to interact with the receptor the virus uses to enter host cells. In other words, which mutations have the potential to make the virus more infectious. Also from lab experiments, we are starting to get an idea of which mutations can impact on the ability of host antibodies to neutralise the virus. In other words, which mutations might help the virus evade the current vaccines, or at least make them not as effective.
What we are now seeing is those advantageous mutations, and combinations of advantageous mutations, appearing in the real world. Importantly, these mutations can arise in any variant in any lineage, if the conditions are right. And in many countries, conditions are perfect right now. The more community transmission, the more chances of variants with different and worrying combinations of mutations arising. In essence, what we are watching is evolution in action.
The more infectious B1.1.7 variant was identified in the UK because of a combination of factors. First, they saw a surge in cases, which could just have easily been caused by everyone going Christmas shopping. Second, some of their testing labs are using a three gene PCR test which it just so happens one of the mutations impacts on making the rise in B1.1.7 cases really obvious. And third, they are leading the world in terms of the amount of genome sequencing they are doing.
In other words, variants with advantageous mutations are likely everywhere, but haven’t been identified yet because no one is looking for them. But those lab experiments have shown us what to be on the lookout for. Rather than focusing on specific “variants of concern”, everywhere with uncontrolled community transmission should be looking for any of the mutations of concern in any virus they see. That means more genomic sequencing, especially in places which are doing almost none and for which we know almost nothing about the variants that are infecting people. This is going to need a global and coordinated effort to ensure every country has access to sequencing.
Meanwhile, lab-based researchers will keep doing their experiments to try to predict which other mutations we should be concerned about and looking out for.
What we urgently need governments and the public to do is everything in their power to stop community transmission so we can try to stop the virus evolving into something even more difficult to control.