We expect that our doctors aren’t being paid by pharmaceutical companies when they prescribe us medicine. Should medicinal cannabis be any different?
You can imagine the outrage. A major pharmaceutical company opens a clinic to prescribe its opioids via online consultations and prescribes pain pills to thousands of New Zealanders around the country.
Now, replace the word “opioid” with “cannabis”. Is it still OK?
The pharmaceuticals industry has long been under scrutiny for conflicts of interest. Last year, Stuff revealed drug companies gave New Zealand doctors, nurses and pharmacists $342,759 in payments or sponsored trips in 2021 alone. In the US, drug companies have been fined billions of dollars for illegally promoting their products and the role of conflicts of interest in the country’s opioid epidemic have been well documented.
So the idea that drug companies in New Zealand could directly own doctors’ clinics seems hard to believe. However, it turns out there’s nothing in law to prevent this happening and it’s a loophole that the country’s nascent medicinal cannabis industry has been exploiting.
Two years ago, a medicinal cannabis company called Medical Kiwi (since renamed Aether Pacific Pharmaceuticals) opened the Pain Clinic, an online doctors clinic that specialises in prescribing medicinal cannabis. It later opened brick-and-mortar clinics in Nelson and Christchurch.
Not long after, another cannabis company, Eqalis (since merged with cannabis company Cannasouth), opened a clinic boasting that patients could have an online consultation and get their cannabis prescription sent to their letterbox without having to leave the couch.
Is it wrong for a drug company to be paying a prescribing doctor’s salary, or is medicinal cannabis a warranted exception?
Mediweed
First, a recap on New Zealand’s medicinal cannabis scheme. When medicinal cannabis was legalised in 2020, the drug was shoe-horned into our medical system.
Medicines have to be approved by Medsafe, and approval depends on the medicine being safe and effective. This usually follows phase-three clinical trials which provide evidence of what conditions a drug may be effective for, in what doses and with what risks. The drugs may then be funded via Pharmac, if it meets a cost-benefit test, so when you get a prescription it generally only costs $5 – the rest is picked up by the taxpayer.
Medicinal cannabis has generally not met either of these thresholds. To date, only two cannabis products have been approved via the normal pathway under the Medicines Act: Sativex for multiple sclerosis when other medications don’t work, and Epidyolex, a CBD oil for specific forms of epilepsy. Neither of these yet receive Pharmac funding.
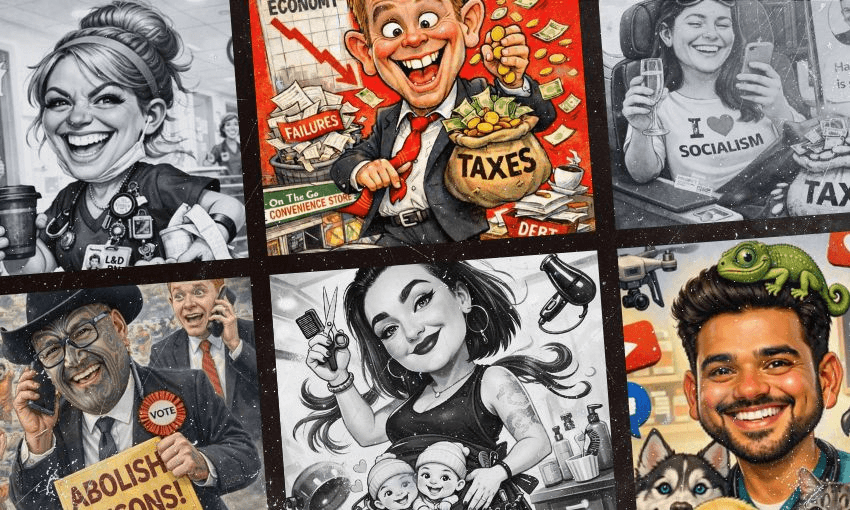
(Photo: Getty Images)
Partly due to decades of prohibition – and the fact cannabis is generally consumed as a plant rather than a sterile pill – research into medicinal cannabis is still at an early stage. Consequently there’s not the kind of gold-standard evidence to prescribe it compared to other prescription pills. And yet thousands of people believe it helps their medical conditions.
Enter the medicinal cannabis scheme. Until 2020, prescribing cannabis required approval from the health minister, which in practice was almost never forthcoming. The medicinal cannabis scheme introduced a kind of work-around of this system to meet the growing demand for legal medical weed. Under the scheme, cannabis can be prescribed as an “unapproved medicine” (meaning it’s not proven to be safe or effective) by any doctor, for any condition. This includes cannabis flower – aka buds – as well as THC and CBD oils and even gummies.
The cannabis products themselves, however, are strictly regulated and have to meet a minimum quality standard – a pharmaceutical standard of safety and consistency – before they can be prescribed. While our prescribing rules are relatively liberal, this standard has been called among the strictest in the world. Getting plant material to conform to a pharma standard has proven exceedingly difficult. Despite 42 companies having licences to grow cannabis, only three have products approved for sale. All three have had to invest tens of millions of dollars to reach that point. The rest of our prescribable cannabis is imported (and even some cannabis sold by local cannabis companies is actually imported).
These tough restrictions have brought the industry to its knees. None have made a net profit to date. All three of the country’s publicly listed cannabis companies are trading at less than 10 cents a share, and one, the aforementioned Cannasouth, is in voluntary administration.
Even when products have been approved, most doctors have been reluctant to prescribe it due to the lack of gold-standard evidence and knowledge about the drug (and probably also the stigma stemming from decades of prohibition).
Enter the cannabis clinics. To serve the growing demand for medicinal cannabis, at least a dozen independent clinics have been established around the country (and online) with doctors who specialise in prescribing it. The rationale is that, unlike your over-worked GP, they have the time to understand things like dosage, drug interactions and the evolving evidence of efficacy of this unapproved medicine. Anecdotally they are also far more likely to dole out scripts.
But then cannabis companies also began opening clinics. While the companies argue they’ve been motivated by these same factors, the clinics are also an important source of revenue for the cash-strapped growers. And it appears to be a clear conflict of interest in our medical system.
A regulatory hole
So how is it possible for a drug company to open a doctors clinic that can prescribe its own products? Surprisingly, a Medsafe spokesperson told The Spinoff that there’s nothing in New Zealand’s laws that prevent a drug company from setting up a clinic that can prescribe its products.
Instead, only the doctors themselves are regulated by the Medical Council, which can investigate doctors who break its guidelines around prescribing and managing commercial conflicts of interest. Breaching these can lead to a doctor’s medical certificate being revoked.
The Council’s conflict of interest statement says doctors decision-making must be “free of actual or perceived bias towards an organisation, device, product, person or service” and that disclosure of commercial conflicts is vital.
However, the guidelines don’t specifically address the sort of direct conflict of interest that arises when a drug company is actually paying the salary of the doctors that can potentially prescribe its medicine. Most of the statement details how conflicts should be managed by strategies like disclosing conflicts to patients and being critical of drug company advertising, rather than prohibiting certain relationships outright. Although the statement does say doctors must not accept payment from a drug company to cover the cost of travel, attendance or meals at an event supported or funded by a drug company, it seems a drug company can still pay their salary.
University of Otago bioethics associate professor Josephine Johnston questions whether this provides sufficient safeguards.
“I don’t think that’s a good strategy for managing conflicts of interest,” Johnston tells The Spinoff. “There’s a lot of evidence that really well-meaning people can be influenced and not know.
“I’m not saying they’re bad people for doing that. I think most of us overestimate our ability to manage things like financial relationships and advertising that influence us.
It’s also very hard to actually prove that someone’s prescribing practices were influenced by a conflict of interest,” she says. “Unless it’s really extreme, it’s quite hard to show there’s actual bias.”
If conflicts of interest aren’t managed appropriately, then the consequences can be significant, particularly if it erodes the public’s trust in the health system, she says. “Once that gets eroded it’s really hard to get it back.”
In the US, doctors clinics have to be owned by doctors, rather than businesses, Johnston says.
A spokesperson for the Medical Council says it regularly reviews its statements and guidance and these could be changed “if specific concerns arise that demonstrate that our statements need strengthening or updating”.
If a member of the public has concerns about a doctor potentially not managing a conflict of interest, they can also submit a notification to Medical Council, it says. It wouldn’t reveal whether it had received notifications regarding concerns about conflicts of interest regarding these clinics, saying these were confidential.
One cannabis company has actually used this conflict of interest as a selling point. A marketing report commissioned by Cannasouth spruiks the benefits of the company owning its own clinic. Under a section titled “RestoreMe: Why it is an important business for Cannasouth to own,” it notes that an Australian cannabis company has been able to increase sales by running a service that refers potential cannabis patients to specific doctors clinics.
“That clinic is not obliged to prescribe Cannatrek product, but the physician will often do so given the relationship that the doctor has with the company”, the report notes. “RestoreMe takes the specialist clinic model to New Zealand”.
It’s important to note that Aether Pacific does not yet have any medicinal cannabis products approved in New Zealand. Cannasouth has three oils and two strains of flower approved, but as mentioned the company is in voluntary administration and its future is uncertain.
Cannsouth did not respond to requests to comment for this story. It’s worth noting, however, that The Spinoff hasn’t seen direct evidence that its RestoreMe clinic favours Cannasouth’s products when prescribing.
Aether Pacific provided a statement that says it manages “any potential, real or perceived conflict by following international best governance practices in having any of our interests in a clinic at arm’s length in a separate company entity”. It says the Pain Clinic has its own board and doctors were able to choose prescriptions “from all available medicines in NZ”.
“In our case the pain clinic is a separate autonomous entity that helps facilitate patient access to locum GPs who can prescribe medicinal cannabis to help patients in need who may not have access otherwise,” the company says.
RegulateMe
The country’s professional body for GPs, the Royal College of General Practitioners New Zealand (RNZCGP), says these safeguards aren’t enough and the loophole should be closed.
“This was a complete political policy to make medicinal cannabis legal that paid no attention to the medical evidence or the normal standards by which we operate,” RNZCGP medical director Dr Luke Bradford says.
“There’s real concern that the clinics are being owned and run by people who are profiting from the production of medicinal cannabis,” he continues. “There needs to be clear separation between the prescriber, dispenser and between the prescriber and the pharmaceutical manufacturer, as you’d expect with any other medicine.”
RNZCGP has also raised concerns about cannabis clinics owning pharmacies that sell the products they prescribe, or dispensing cannabis products directly. This month RNZ reported that the country’s largest cannabis clinic had opened a new premises and pharmacy on Auckland’s North Shore. Traditionally doctors haven’t dispensed medicines to avoid a conflict of interest whereby they profit from prescribing drugs.
But is it such a big deal if a conflict of interest leads to doctors prescribing more medicinal cannabis than they might otherwise? After all, if just another 1.6% of people voted in favour of the recreational cannabis referendum in 2020, then anyone could buy cannabis for any reason. Surely allowing people to access cannabis that has met a strict safety standard from a doctor is better than people buying weed from a tinny house down the road?
Bradford says this argument ignores the ethical foundations of the medical system, which we weaken at our peril. “We’re not drug dealers,” he says. “They shouldn’t be doing it through a doctor. We should have either had medicinal cannabis better regulated and insisted it was an evidence-based medicine like every other medicine, or legalised cannabis for recreational use. But we shouldn’t be using the facade of medical responsibility to allow people to access cannabis for recreational purposes.”
Given the lengths Big Pharma companies have gone to influence doctors prescribing decisions, it seems surprising that none have opened doctors clinics before, given it’s completely legal.
However, Josephine Johnston says most other drugs are publicly funded, which involves extra layers of regulation to ensure the government’s getting value for money. Because medicinal cannabis doesn’t receive public funding, it seems to fall into a regulatory gap.
Bradford says there’s not really a market for a clinic focused on drugs that are already being bought and subsidised by the government. It’s also easier to tell if other drugs are being over-prescribed.
“There is very clear evidence on what you can and can’t use opioids for and therefore you could be held accountable very easily for improper prescribing,” Bradford says. “There is very limited evidence on what medicinal cannabis is useful for.”
Unlike medicinal cannabis, it’s also hard to see any public demand for a Big Pharma clinic when their drugs are already widely available. And if they ever tried, there’d probably be picketing in the streets.