Māori have fared worst in every pandemic New Zealand has seen. Measures must be taken to ensure equity during the Covid-19 outbreak or history will repeat, writes public health physician and senior lecturer Dr Rhys Jones.
Covid-19 is about to hit Aotearoa in earnest. The New Zealand government’s response to date has generally been received positively, but we know the worst is yet to come. Our nation’s preparedness and ability to respond effectively will be sternly tested over the coming weeks and months.
Nowhere will this be brought into sharper focus than in relation to Māori whānau and communities. Many Māori health professionals are extremely concerned about the likely disproportionate impacts on Māori, and about the lack of an effective strategy from the government and health sector to deal with these impacts.
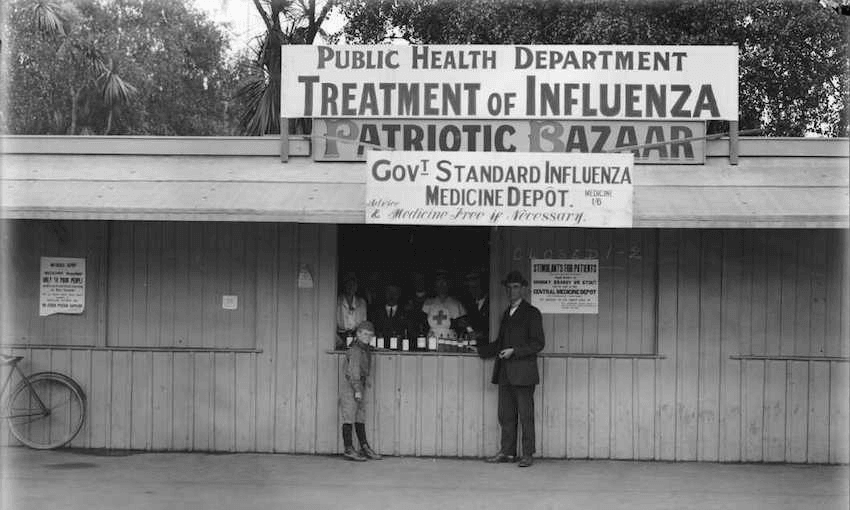
History paints a grim picture with regard to the impact of previous pandemics on Māori, providing a clear warning of what could lie ahead if we don’t take appropriate action. The 1918 influenza pandemic resulted in a death rate for Māori of 4.2%, approximately seven times as high as the non-Māori death rate. In the 2009 influenza A (H1N1) pandemic, rates of hospitalisation and death were also much higher for Māori than for other ethnic groups.
Why do Māori appear to be at greater risk from pandemics than many other ethnic groups in New Zealand? There are many different factors at play, including underlying social and economic disadvantage as a result of historical and contemporary colonisation, a greater burden of chronic diseases that increase the risk of more serious outcomes from infections such as influenza, and poorer access to and quality of health care.
But inequitable outcomes can also be attributed to the failure of the government to respond to pandemics in a way that adequately protects Māori communities.
One of the stated goals of the NZ Influenza pandemic plan is to “minimise the impact of the disease and to mitigate its effects on the people of NZ without increasing health inequalities.” However it is clear that the current pandemic response, if it continues under a business-as-usual model, will preferentially benefit Pākehā New Zealanders and fail to protect Māori from the worst outcomes.
How do we know this? We need only to look at the existing health system, which consistently delivers poorer quality care for Māori, to understand the default setting for health-related interventions in this country. The report of the first stage of the kaupapa inquiry into health services and outcomes found pervasive inequities that were inconsistent with the government’s obligations under the Treaty of Waitangi. It highlighted institutional racism, “anti-equity” funding arrangements and a lack of accountability for health entities in relation to equity for Māori.
There is a real danger that these systemic failures will be repeated in the current response to Covid-19. The Ministry of Health’s strategy lacks a Treaty partnership approach and has little to suggest it is appropriately addressing glaring equity issues. The government’s $12.1 bn package to support New Zealanders, while including a benefit increase and a doubling of the Winter Energy Payment, does not do enough to protect those in greatest need. Why, for example, is the government not using the funding boost to implement the recommendations of the Welfare Expert Advisory Group?
A pandemic strategy that relies on existing leadership and structures, and utilises conventional approaches, will fail to achieve equitable outcomes for Māori. It may work well for those it has been designed to work well for – predominantly middle-class, Pākehā New Zealanders – but will leave many others to fall through the cracks.
So how do we stop this happening? First and foremost, there must be Māori governance and leadership at all levels of the pandemic response – nationally and within DHBs, as well as across all other sectors. Iwi, hapū, whānau and Māori communities are mobilising, but this needs to be supported and linked to the appropriate information, resources and infrastructure.
Critically, every aspect of the pandemic response needs to have equity at its centre. It must ensure that all our communities have the resources to be able to carry out public health measures to prevent spread of the virus. For example, how do we make sure effective handwashing is possible among whānau in remote communities in Northland with severe water shortages after a summer of drought? What is being done to support Māori in precarious employment to be able to take time off work to self-isolate and still have enough money to put food on the table?
Every decision must be reviewed with respect to its impact on equity for Māori and adjusted accordingly. For example, what measures are in place to ensure essential supplies are available in the most vulnerable communities? As health care resources are diverted to manage Covid-19 cases, what existing services will be cut? Will Māori and Pacific peoples, once again, be hardest hit? If it comes to the point of hospitals having to prioritise people for intensive care beds or ventilators, how do we ensure that Māori are not disadvantaged?
It may seem like these are luxury considerations when we’re in the middle of a crisis. But if these issues are not addressed the process will default, once again, to inequity.
That leaves many of us with grave concerns about the response to Covid-19 – that it will reproduce racist outcomes and end up being another chapter in the long history of health-related Treaty breaches. We must not let that happen.
Dr Rhys Jones (Ngāti Kahungunu) is a public health physician and senior lecturer at Te Kupenga Hauora Māori, University of Auckland.