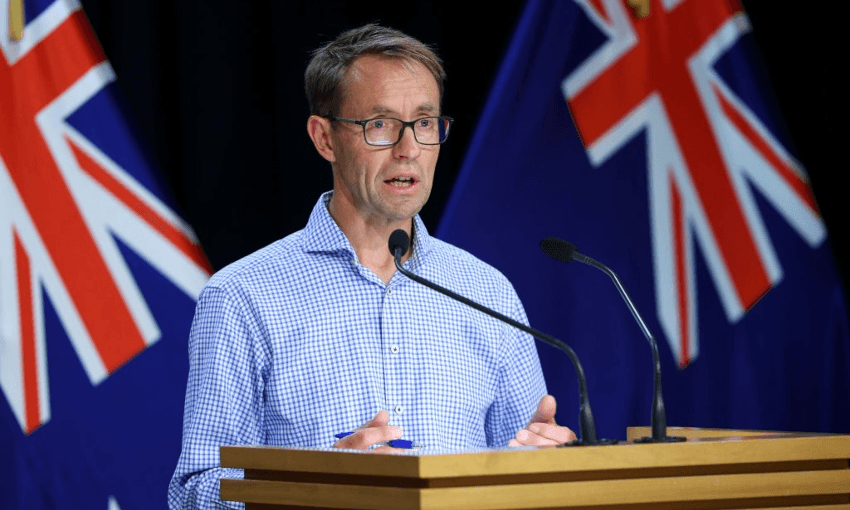
There have been 11 more deaths from Covid-19, bringing New Zealand’s pandemic death toll up to 221 and the seven-day rolling average of reported deaths to 10.
Of the 11 deaths being reporting today, two people are from the Auckland region, two are from Bay of Plenty, six are from Waikato, and one is from the Wellington region. Two of these people were in their 50s, one person was in their 70s, four people were in their 80s, and four people were in their 90s.
Six were men and five were women.
Once again, hospitalisations have dropped. There are now 913 people being treated with Covid-19, including 28 in intensive care.
Speaking from the Ministry of Health, Ashley Bloomfield said this was “quite a drop” on yesterday. The decrease was mainly in Auckland, said Bloomfield, where hospitalisations have dropped to 514 down from 576 yesterday. There are now 148 people in North Shore hospital, 207 in Middlemore and 159 in Auckland. “This fits with the drop in cases we’re seeing there,” said Bloomfioeld.
There are 18,423 new community cases. In the seven days to March 20, there were 24 new cases per thousand in the country, compared with 27 per thousand the day before. However, the DHBs with the highest rates are Tairāwhiti (44 per thousand) and Hawke’s Bay (38 per thousand).
Auckland has registered another drop in new cases, with 3,629 today. That’s still the highest regional count nationwide but Canterbury is close behind – 3,150 cases were confirmed there overnight.
It’s also clear cases are increasing in the South Island, said Bloomfield.
Māori have the highest rates of infection at 35 per thousand, then Pacific at 28 per thousand. NZ European and Asian ethnic groups are currently at 21 per thousand. There has been a decrease in the number of cases reported among Māori for the week to March 20, but hospitalisations have increased.
In Tairāwhiti, Māori case rates are the highest in the country, at around 112 per thousand.
Bloomfield said delivery of the vaccination programme was “as high as I might have aspired to but higher than I might have expected”. There is now ongoing work to make sure there can be even more equitable access to vaccinations, particularly for Māori children. “Māori parents were more likely to wait for a bit until they got [their children] avccinated, I think they wanted assurances around safety.”
Health officials did know how to talk with Māori, said Bloomfield when asked to admit they did not.