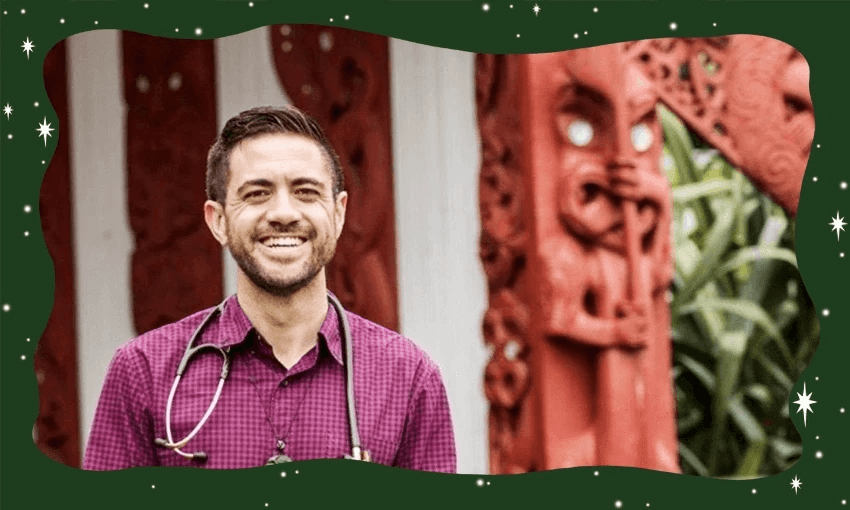
With the new government pledging to scrap the Māori Health Authority, board member Dr Mataroria Lyndon tells Ronan Payinda that while the exact path forward may not yet be known, there’s no stopping the fight for Māori health equity.
Dr Mataroria Lyndon (Ngāti Hine, Ngāti Wai, Ngāti Whātua, Waikato) is a senior lecturer in medical education at the University of Auckland, co-founder of Tend Health, and board member of Te Aka Whai Ora – Māori Health Authority.
Mataroria credits te reo and tikanga Māori as his tūāpapa – the underpinning of his identity and career successes, passed down to him by his elders. Amid growing disquiet over the coalition government’s approach to Māori issues, I spoke to him about the future of Māori health in Aotearoa.
We’ve been hearing a lot about the new government’s plans to abolish the Māori Health Authority. If Te Aka Whai Ora is disestablished, what is the path ahead for Māori health?
Māori health still very much remains. Whether we have Te Aka Whai Ora in place or not, future governments will still need actions to address health inequity for Māori. The work of Te Aka Whai Ora has been about how Māori can have greater decision-making and authority over hauora Māori – giving Māori autonomy over setting strategy and policy and commissioning of Māori health services, and monitoring the outcomes of the health system.
It is up to the government to lay out their view of the road ahead, but in terms of the important mahi, both Māori and non-Māori allies will carry forward the aspirations and the vision for Māori health equity and wellbeing into the future.
Can you explain the core reasons behind why Te Aka Whai Ora was established in the first place?
The 2019 Waitangi Tribunal report into health services for Māori was a game-changer. It identified a number of inequities for Māori – the lack of decision making, lack of accountability and monitoring, inequitable resourcing, the under-representation of Māori within the health sector workforce. The tribunal stated that these inequities were breaches of Te Tiriti and it recommended the creation of a Māori health authority.
Secondly, the 2020’s health and disability system review recommended a Māori health authority as well. So these reports are one basis, alongside many pioneers and health leaders in Māori health that had been calling for a Māori health authority over the last few decades.
We’ve had decades of work by Māori health advocates calling attention to the need for a Māori health authority. Those reasons haven’t gone away, have they?
Alongside those reviews and reports, the health inequities still remain. And the aspiration and the work continues, irrespective of whether there is a Māori health authority or another entity to address these issues.
What I would also like to highlight is the iwi-Māori partnership boards established by the Pae Ora legislation. They have a key role in reflecting whānau voice within the health system, as well as monitoring the performance of health services in their localities. Even if Te Aka Whai Ora is disestablished, iwi-Māori partnerships are another mechanism of Māori health leadership.
I don’t know personally what the road ahead will look like – that’s ultimately the job of the new government. But I know that iwi decision-making in the health system is here to stay.
With decades of work and advocacy, why are inequities still here? Why are they so entrenched in our health system?
One of the core reasons is the wider social determinants of health. But we know that it’s not just socioeconomic factors alone, because Māori still have worse health outcomes even within the same deprivation brackets as non-Māori.
So there is an analysis around poverty, income, employment, education, but that’s only part of the issue. We also need to look at the health sector – there are inequities in access to care, quality of care, and the under-representation of Māori in the health workforce.
And then we also need to look at the health system level. The Waitangi Tribunal found a lack of Māori decision-making, a lack of accountability for Māori health, in our health system.
These are just some of the issues that have been identified. But there has been progress made, such as through the likes of the Māori and Pacific Admission Scheme (MAPAS) programme, there has been increasing numbers of Māori students and graduates coming through. But the issue still remains, and the job now is to keep going.
You were brought up in Whangārei and in South Auckland. Here in Te Tai Tokerau Northland, there’s a disproportionately high health need, especially among our Māori communities. How did your upbringing influence your advocacy for Māori health equity and your career direction?
My parents were a big inspiration to me. When I was young, my mum, who had a teenage pregnancy, went back to school to get her high school certificate, and I was a kid going along with her. There was always a sense instilled from my parents of wanting to get a good education, wanting to do better for their family, for their whānau, their tamariki.
But always remembering our roots, of being from where we’re from, who we are, of growing up in te reo Māori – my dad’s first language that he passed onto us. Te reo Māori is an important connection to our whānau, to our whakapapa, and that’s something that I’ve always been able to take forward with me in the work I do.
We moved around a lot growing up because my parents were always finding work. Coming back to South Auckland, which is where my dad was teaching, where I went to school at Tangaroa College, it was an example to me about different communities. Whether that be rural Northland where we whakapapa to, or deep in South Auckland, in a heavily Pasifika and Māori community, a high-needs community – seeing what those different needs were was a good experience during my upbringing.
I’ve worked previously across the health sector, from a frontline doctor, a DHB board member, and now as a Te Akai Whai Ora board member. These different experiences, alongside my own upbringing, made it clear to me that we need to address Māori health inequity.
Some people don’t see the need for Māori health programmes because they think the impacts of colonisation on our health system are long in the past. Can you explain why there’s still a pressing need today?
Having a one-size-fits-all approach is not a good way to address health inequities or differences in health needs – that’s one explanation for why Te Aka Whai Ora was put in place, to identify solutions that work for Māori.
Secondly, it’s not a level playing field when it comes to everyone’s health. There’s an assumption that if the health system is just based on need alone, then we’re all going to have the same health outcomes.
But we know that because of the issues around poverty, housing, education, employment, income – those necessities that people need to lead healthier lives – these aren’t the same, particularly for Māori. It’s not a level playing field, hence the need for more targeted support and action to tackle these health inequities.
We need to acknowledge that the health system was constructed to benefit some more than others. That’s why there’s a need for greater Māori decision-making, design and delivery of our health services.
There is a saying that what works for Māori works for everyone. I’ve seen that throughout my career. With the Māori health team at Counties Manukau DHB, we held hapū wānanga on marae for pregnant mums and whānau. And there were non-Māori accessing that marae programme as well, because they really enjoyed the Māori approach of whanaunga, having it in a marae-based setting, connecting to whānau.
And we saw the same for Covid outreach done by Māori health services – we had iwi health services running vaccination programmes across New Zealand. Many iwi health services probably vaccinated more non-Māori than Māori, because it was a service that went out to the community and was open to everyone.
All these examples show that when Māori have decision-making and accountability over their own services, they’re effective at bringing healthcare to our communities. But Māori health services are also still open for others to access as well. So when we fight for Māori health equity, we’re also going to uplift all of Aotearoa.