With hundreds of testing alternatives available, it is crucial that we pay close attention to what is in play, and which are most effective. Siouxsie Wiles guides us through them.
I was blown away to discover that there are more than 500 different tests for Covid-19 either in development or already commercially available.
The Foundation for Innovative New Diagnostics (Find), based in Switzerland, has started pulling together a list of all the tests currently available around the world. As of yesterday their list included a staggering 545 results. They fall into five different categories: “immunoassays”, “molecular assays”, “sample collection/inactivation”, “digital solutions”, and “other diagnostics”. The vast majority of the tests fall into one of the first two categories, and most of those are already commercially available.
Immunoassays versus molecular assays
I’ve written about immunoassays and molecular assays before. Molecular assays are the tests that look for the genetic material of the virus. These are very specific and very sensitive, but only work when someone is shedding the virus. This is the type of test we are doing here in New Zealand. People get swabbed, and then those swabs are sent to one of several labs around the country. Together they can process thousands of samples each day.
There is now at least one company in the US that is offering a version of this test that can be done in just a few minutes. It’s based on pretty much the same technique but using a miniaturised version of the lab equipment so it can be run anywhere. The only snag is that it just runs maybe one or two samples at a time. The company already had a similar test for influenza and a few other diseases, so they’ve just adapted it for Covid-19. I haven’t been able to find any information on how reliable it is but did read that that some doctors have raised concerns that they are seeing patients who have all the symptoms of Covid-19 but test negative using the machine.
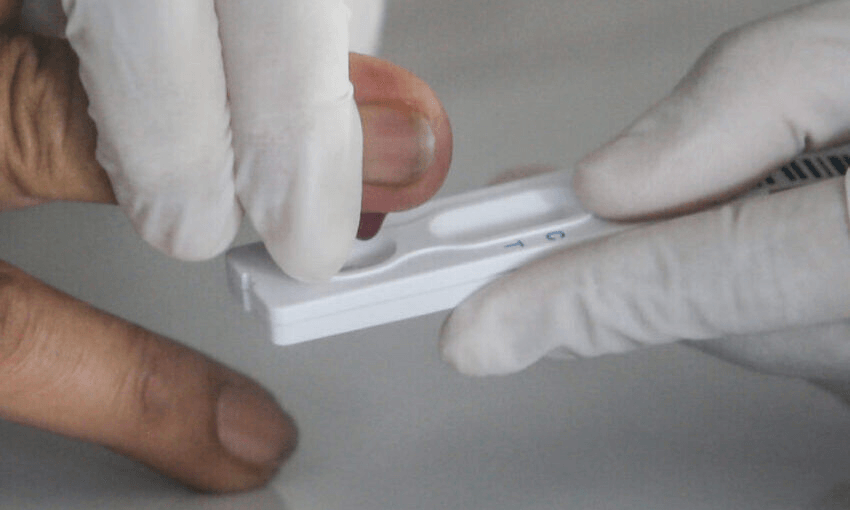
Immunoassays are made up of two types of tests. The first uses antibodies to detect specific proteins made by the virus. I haven’t seen these in use yet. The other looks for our body’s response to the virus. These are also known as serology or antibody tests. When people are tested is absolutely crucial for immunoassays – too early in the infection and there won’t be any antibodies to detect. Another issue is that not all infected people produce detectable antibodies. So, at the moment it’s not clear how sensitive or reliable the home-use versions of these tests are. But they are much cheaper and faster than the molecular assays and can tell whether someone has already had Covid-19. That’s why there is so much interest in using them overseas. That doesn’t mean they are always worth leaping at, however. Both the UK and Spain spent millions of dollars buying serology that proved too unreliable to use. Here Medsafe is reportedly considering restricting the importation and sale of such tests.
Testing the tests…
With backing from the World Health Organisation, the Switzerland-based Find is offering to put each test on their list through its paces on a voluntary first come, first served basis. Find has access to archived samples from 150 people – 50 who had Covid-19, as well as 100 who didn’t. Their labs will run each test against those same 150 samples alongside their “gold standard” test to see if it can pick up all the positives as positives and all the negatives as negatives. Once the material from the 150 people is all used up, they’ll get samples from another 150 people and keep testing. They are posting the results up on their website as they go along.
So far four molecular assays have been evaluated. They are all tests that work by looking for the genetic material of the virus. The results are available here. It’s interesting to observe that these particular assays test for a range of different viral genes with differing limits of detection. Most of them can measure down to 1-10 copies of the gene per reaction, whereas one can only test down to 10-50 copies of the gene per reaction.
The good news is that all the tests picked up all the positive samples. That means there weren’t any false-negatives – samples that were flagged as negative but were actually positive. This is a very good thing. It’s worth bearing in mind, though, that a crucial factor for when the tests are used in the “real world” is how well the person is swabbed to get a virus sample. Around the globe, doctors are seeing patients who have all the symptoms of Covid-19 but end up testing negative. If those patients really do have Covid-19 but are treated like they don’t then that could be disastrous. That’s why here in New Zealand we count both probable and confirmed cases together.
As for false-positives – when a negative sample returns a positive result – three of the four tests identified between one and four of the negative samples as positive. Find say these need to be further investigated but they are less concerning from an infectious disease perspective than false-negatives
.
A dashboard for all independent data
As well as doing their own evaluations, Find have also set up a website to publish all the data that other independent labs have on how the different tests perform. This is really important. It can be very tempting for some companies to rush a crappy test to market in an attempt to maximise profit from the pandemic. This way, anyone can see how the tests perform and decide which ones they want to invest in using. This is especially critical for those countries, districts, or hospitals with limited capacity to carry out their own independent evaluations.
Given the experience of Spain and Britain, I’m looking forward to seeing how they immunoassays do when they are put through their paces. According to the dashboard, just two of the roughly 20 immunoassays approach the threshold for being both sensitive and specific. As New Zealand’s elimination strategy bears fruit, the calibre and reach of our testing is crucial, and as in so much of our response, we need to keep a close eye on what is happening overseas.