With over 24 million confirmed cases and more than 820,000 people dead, Covid-19 is playing out differently in various parts of the world. To understand this a little better, Siouxsie Wiles and Toby Morris walk you through the Covid-19 ‘triangle’.
Since this pandemic started, I’ve been getting lots of messages from people and hearing an awful lot of pundits who sum up Covid-19 as a simple case of virus vs person, with a binary outcome: the infected person either lives or dies.
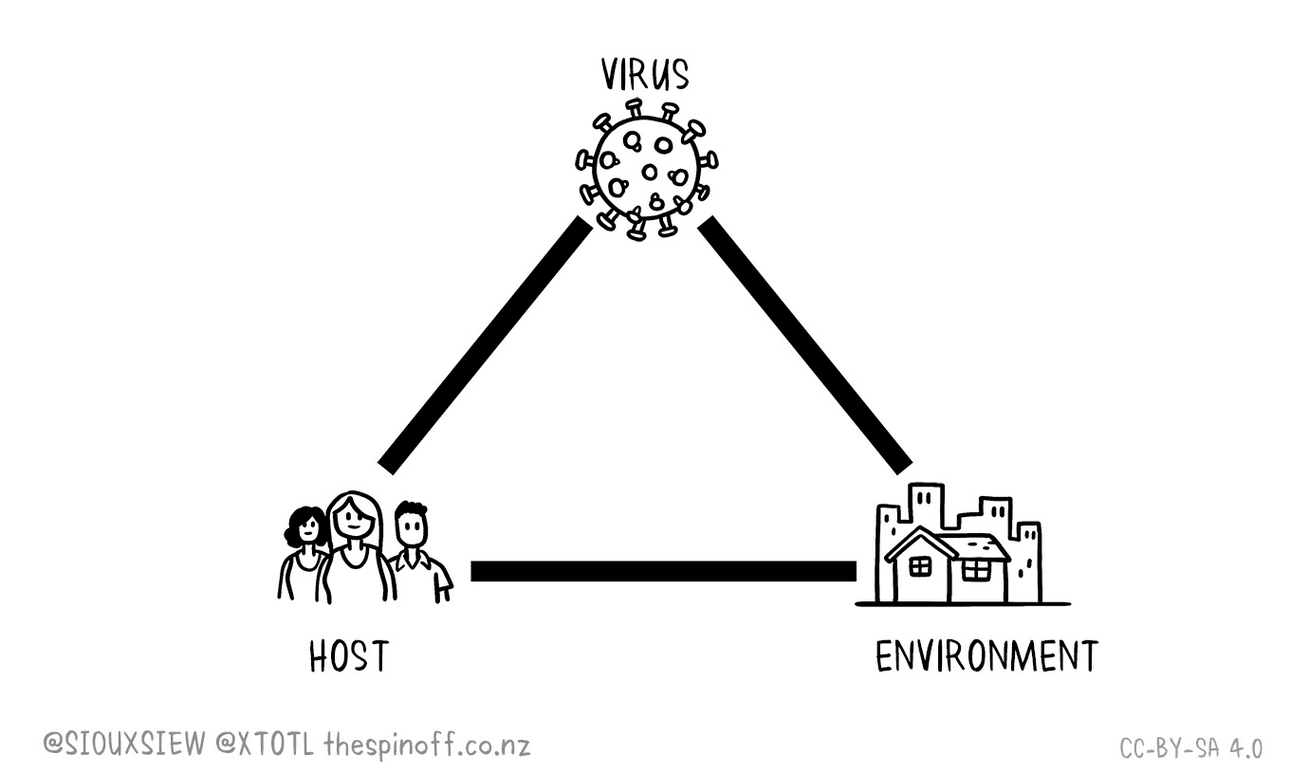
If only it were that simple, but there’s more to it than just the microbe against its unfortunate host – there’s also what I’ll call the “environment”. Together, these factors make up the disease triangle. It’s the differences between these factors in any given place or situation that are giving us the dynamic pandemic the world is currently experiencing. Let me explain.
The microbe
While viruses and bacteria have their own names, like humans they can come in different varieties. And sometimes those varieties can differ in how infectious they are or how much damage they can do to us. The influenza virus is a good example of this. There are actually four species of influenza virus and lots of different subtypes within them. They mutate on a regular basis as well as mix and match with each other. In early 2009, a strain called H1N1 emerged and caused a global pandemic. H1N1 was found to cause more breathing difficulties in young healthy people than the normal seasonal influenza strains which are most dangerous for older people.
Toby Morris and I recently explained how the virus responsible for Covid-19 has mutated so that there are now different varieties, or lineages, circulating around the world. Having this information is now helping us link cases in a cluster or see where an imported case might have come from.
If you need a reminder, the virus’ genetic material is a strand of RNA made up of almost 30,000 nucleotides. These code for the amino acids that in turn give us the proteins that make up the virus. Each time the virus enters a new cell and replicates, its genetic material is copied, and nucleotides can get replaced by mistake. It looks like we’re seeing roughly two nucleotide changes happening a month for the Covid-19 virus which means its mutating quite slowly.
At the moment I’m not aware of any good evidence that the virus is becoming more or less deadly. But there is one mutation that’s quite interesting. At some point early in the pandemic, the adenine nucleotide at position 23,403 changed to a guanine. Strains with that mutation have now spread around the world. Does this mean that mutation makes the virus more infectious? Possibly. The mutation changes the amino acid at position 614 of the spike protein from an aspartic acid (referred to as D) to a glycine (G), which is why it’s called G614.
Researchers have shown that virus-like particles engineered to contain the G614 version of the spike protein are better at entering laboratory-grown cells than the original D614 version. But the spread of G614 around the world could also be related to the fact that the mutation emerged early in the pandemic in Europe, and travel from Europe spread the virus to many other countries, including the USA. Now this variant is established in the USA which is seeding infections in other countries.
The host
The Covid-19 virus infects people. We are its host. And as hosts, we differ in a lot of ways too. There are genetic differences and age differences. There will be hormonal differences based on whether we’re men, women, transgender, or non-binary. We eat different diets and live different lifestyles. Some of us drink or smoke. Some of us have underlying health issues. We live different lives, have different jobs, and earn different incomes. Any of these things may turn out to influence whether we get Covid-19 and if we do, how the disease plays out in us.
As more people get Covid-19, more studies are being published about what the virus can do to us. Some of these studies are small and may not end up being correct once more data comes in. But here is just a glimpse of what’s being proposed at the moment: it looks like Covid-19 is deadlier as you get older and if you have diabetes, hypertension, COPD, coronary artery disease, and chronic kidney disease. And if you smoke and are male.
Of course, it’s not just about dying. Doctors have found evidence of heart damage in some patients and are really worried about what that might mean for their future health. Others are worried that the virus might worsen diabetes for some patients or even cause diabetes in others. On top of that, there are more and more reports of people who experiencing months of persistent symptoms. These “long haulers” may suffer anything from fatigue, shortness of breath and achy joints, to a racing heartbeat and struggling to think clearly.
So, we know that Covid-19 has the potential to be deadly and may also cause medium and long-term health issues. But we also know that the factors that make some people more or less likely to be impacted will differ between communities within a country, as well as between countries. Some countries have younger populations, others have more people with diabetes. In some countries, many people live with intestinal worms that influence how their immune systems respond to other infections. In summary, we’re a diverse bunch of humans.
The environment
The last factor to consider is the environment. This can include what activity people are doing or the environment they’re in that exposes them to the virus. So were people at a church service, a restaurant or working in a cold store? Do they live with lots of other people or on their own? The environment also stretches much further. It takes in the local and national scale too. What access do people have to healthcare and sick leave? Are the hospitals state-of-the-art and fully staffed with plenty of capacity? Or are they already at full capacity even without a pandemic? Is there even a local hospital? Do people have a culture of working for the collective good or is it all about the individual? Is the country experiencing civil unrest, political upheaval or natural disaster? What resources can or will the government supply its frontline workers? Again, some of these things will impact different communities within a country as well as be a big difference between countries.
The Covid-19 triangle in action
Hopefully you can now see why the pandemic is playing out differently for individuals, communities, and countries. Covid-19 doesn’t exist in a vacuum. Instead, the different parts of the ‘triangle’ interact together, changing the risk of cases growing exponentially and of how bad the outcome will be for those infected. I think it’s fair to say though that it’s people and the environment that are playing the biggest role when it comes to Covid-19. What I hope we’re learning is that those are the sides of the ‘triangle’ we need to pay more attention to, to ensure we come out of this pandemic better able to face the next one.