The extraordinary pace of the vaccine development for Covid-19 has nothing to do with shirking safety, and a lot to do with resources. Siouxsie and Toby explain the super highway principle.
The Spinoff’s ongoing Covid coverage depends on support from members. Learn more here.
One of the questions I get asked a lot is this. How were the Covid-19 vaccines developed so quickly? Here Toby and I explain.
Everyone has probably heard that it takes anywhere between five to 10 years, maybe even longer, to get new medicines and vaccines tested and approved. Yet within a year of Covid-19 bursting on to the scene, several new vaccines are in use around the world. According to the Johns Hopkins Covid tracker dashboard, over five billion Covid-19 vaccine doses have been administered to date. So what’s different about Covid-19? Two words. Pandemic and money.
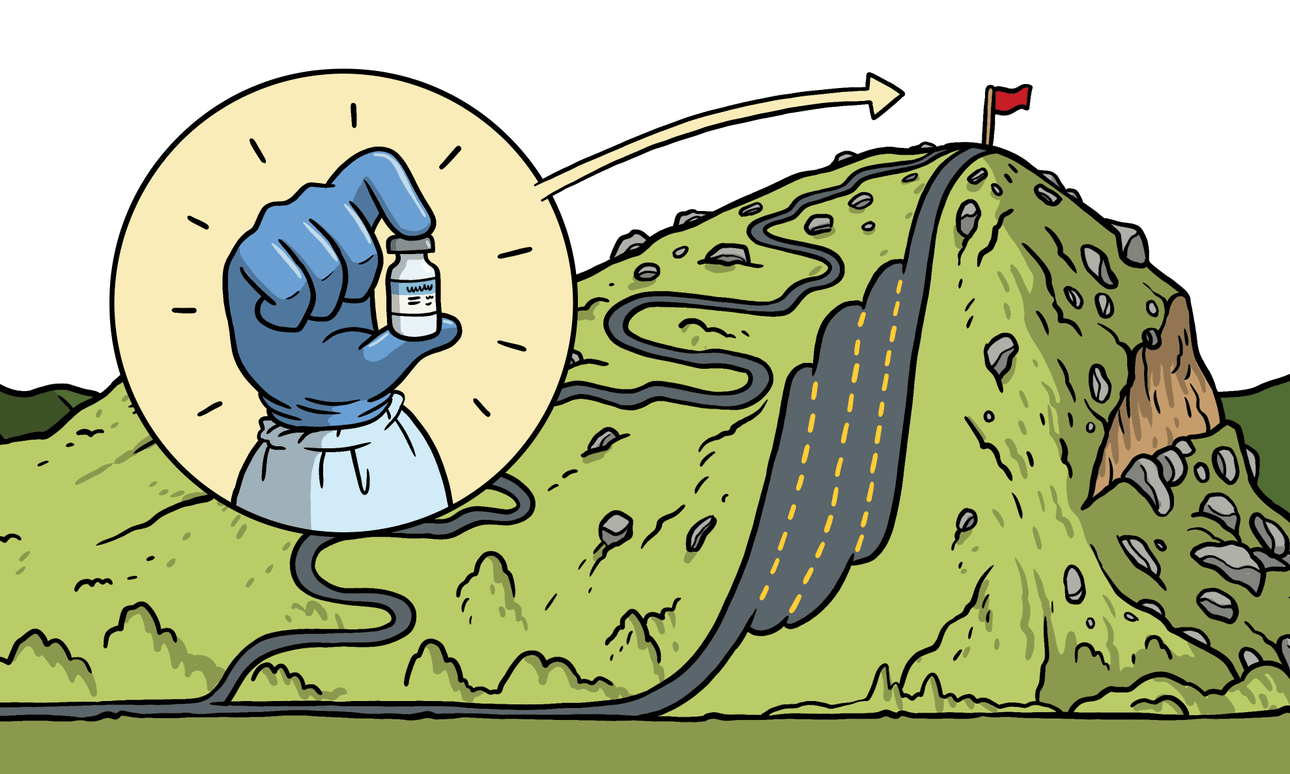
The Covid super highway
The journey from lab to clinic is generally a long and winding uphill road. Before approval in humans, medicines and vaccines have to go through three phases of human clinical trials. A phase 1 clinical trial usually involves a small number of people who are given the medicine or vaccine at different doses, to find out if it is safe and whether there are any common serious side effects. A phase 2 trial involves more people, again looking for common side effects, but also looking to see if there are hints it might be working. If everything looks good, then it progresses into phase 3 trials. Here the number of people vaccinated increases into the thousands or tens of thousands and we start to get information on whether the treatment might actually work. The length of the trials will depend on what the treatment is for, how long it’s likely to take to see an effect, and how easy it is to get enough people enrolled onto the trials.
Normally the different phases of the clinical trials are held one after the other with big gaps in between while people analyse data and work out how to pay for the next phase. Clinical trials are expensive, so companies will likely cut their losses after phase 1 or phase 2 if things aren’t looking promising enough. Once a medicine or vaccine gets all the way to the end of phase 3 trials, the next big hurdle is getting regulatory approval. At that stage the company hands over all the data from the preclinical and clinical trials for the regulators to evaluate. That evaluation can take a lot of time.
Once approved, manufacturing of the newly approved product can be ramped up in preparation for delivery and distribution. Companies would be taking a big financial risk in ramping up manufacturing a medicine or vaccine if there was a chance it wasn’t going to be approved. So you can see why that’s not the norm.
What we’ve seen with Covid-19 is that the long and winding road to approval has been turned into a super multi-lane highway. Instead of running the trials one after the other with long gaps in between, they’ve been run staggered and in parallel. As soon as there was enough information from the phase 1 trials to show safety, the phase 2 trials started alongside them. Then as soon as there was enough info from the phase 2 trials, the phase 3 trials started. With it being a global pandemic there was no shortage of people willing to enrol.
Alongside all that, two other really important things happened. The first is that all of the documentation was provided to regulators as the trials were happening so it could be evaluated on a rolling basis rather than waiting till the end. It’s worth noting at this stage that many of the Covid-19 vaccine trials will carry on for the next few years. That’s to see how long people’s immune responses will last. The second important difference is that manufacturing started before vaccines were approved. This meant that as soon as the vaccines able to be used outside of the clinical trials, there were doses available to be rolled out.
Governments, NGOs, and philanthropic organisations have all poured in heaps of money to help fund the research, the trials, and the manufacturing of several vaccine candidates before they were approved. They took on a lot of the financial risk of the vaccines not making it all the way through the process.
The fruit of decades of research into viruses, mRNA, and lipid nanoparticles
I think it’s worth remembering that before any vaccine or treatment gets to the stage where its ready to be tested in people, there have usually been decades and decades of lab-based research followed by what we call preclinical trials. Preclinical trials use laboratory animals to try to give an indication of how safe and effective the treatment might be in humans.
Covid-19 has been no different in this respect. We’re all benefitting from decades of fundamental research into viruses carried out at universities and research institutions around the world. We’re also benefitting from all the research into deadly coronaviruses which began after SARS appeared in 2002. SARS stands for Severe Acute Respiratory Syndrome and is caused by a similar coronavirus to the one responsible for Covid-19. SARS was followed in 2012 by MERS – Middle Eastern Respiratory Syndrome – caused by a different but related coronavirus, so we’re benefitting from research carried out on that, too.
Of course, it’s not just the decades of virus research that we’re benefitting from. When it comes to the Pfizer-BioNTech mRNA vaccine currently rolling out around Aotearoa, we’re benefitting from decades of research into mRNA and lipid nanoparticles. There’s a great article in Nature highlighting some of the incredible milestones in those fields. They start with the discovery of mRNA in 1961 and the development of liposomes (basically fat balls) in 1965, then putting mRNA into lipid nanoparticles (really really really tiny fat balls) in 1989, all the way to US FDA approval of lipid nanoparticles to deliver various medicines in 1995, 1996, 2000, 2012, 2015, 2017, 2018 … You get the picture.
So while the process of getting the Covid vaccines through clinical trials has been fast, no corners have been cut in safety and scrutiny, and they are based on decades of research. Wouldn’t it be amazing if we could do this for other crucial medicines and vaccines?