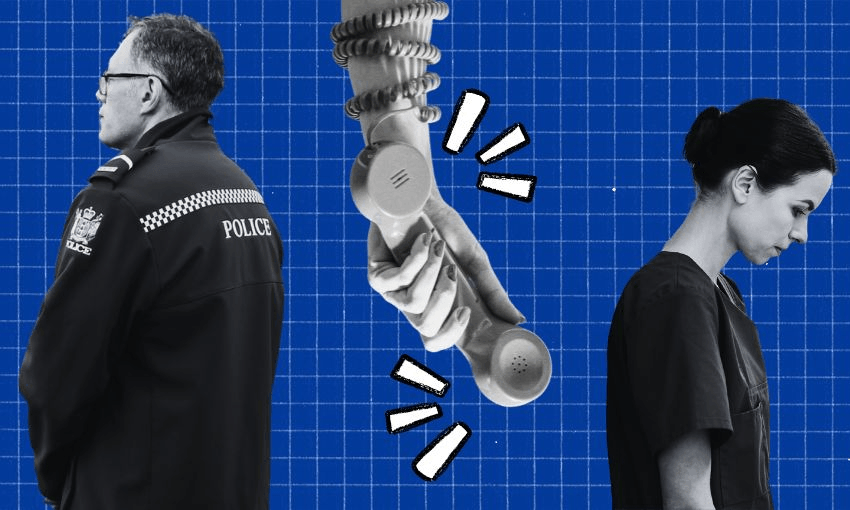
Police have begun gradually reducing their response to mental health callouts, with health staff expected to step up. Here’s what you need to know.
The changes to police’s mental health response, led by NZ Police, the Ministry of Health and Te Whatu Ora, were revealed at the beginning of 2024, and will be implemented in phases over five years. Police have already confirmed the first four stages, to be completed between now and September 2025, which will involve gradually lessening the resources and time spent at low-risk and crimeless mental health callouts, with the end goal of the first year being police only needing 15 minutes to handover patients to emergency department (ED) staff. A health-led response is expected to pick up where police left off.
The first phase began this month, with the introduction of higher thresholds for mental health transportation requests and attendance at mental health facilities before police agree to get involved, as well as police reducing the time spent on voluntary mental health handovers (where people ask to undertake a mental health assessment with health professionals). Police emphasise they will still attend incidents where there is an offence or an immediate risk to life or safety.
Why are police doing this?
To reprioritise where the police are spending time and resources to focus more on instances that pose immediate risk to life and safety, in order to “relieve demand pressures”, they say. According to police data, attending mental health-related incidents made up 11% of all callouts in the 12 months to May 2024, a figure that has risen by 64% over the last five years.
In August, then police commissioner Andrew Costner said the force received a mental health-related call every seven minutes, which he said took up “about half a million hours of police frontline time per year”, and only 5% of these calls had a criminal aspect. “It has been clear to me for some time that this is simply not sustainable and prevents us from keeping other areas of the community safe,” Costner said in a statement. “It impacts our ability to deliver core policing service.”
Reducing the “criminal justice response to many mental health-related calls” also aligned with Kia Manawanui, the whole-of-government plan for mental wellbeing, and would “minimise trauma and coercive treatments”, said a police briefing sent to the minister of police in July. “Most persons in distress do not want police to attend their event unless it is absolutely necessary,” said the briefing. “People experiencing mental distress deserve to have the right people helping them.”
While acknowledging that reduced attendance could “create a reputational risk that Police is perceived not to care”, it was rarely the best agency to respond to a mental health event, said the briefing. “Limiting Police-led responses can have a positive impact by reducing the stigma of mental health and avoid inadvertently criminalising a health event. Additionally, it will likely result in increased Police visibility in the community, contributing to a greater perception of safety.”
What are the next stages?
The second phase, originally planned to commence in January 2025 but now delayed until March, will see 60-minute ED handovers, with police leaving hospital emergency departments within an hour of transporting a person detained under the Mental Health Act. A tightening of mental health custodian rules will also be introduced to ensure those in distress are not needlessly assessed in police custody.
The third phase, originally planned for April to June, is a higher threshold for responding to requests from health practitioners,, and a rejig of handling of reports of missing mental health patients. On the latter change, police said these reports generate more immediate attention than other missing persons reports, and police will work with agencies to establish a new approach that will include the police not being the first to begin a search.
The fourth phase, planned for July to September, will see ED handovers reduced to 15 minutes, and a reduced response from frontline officers to welfare check requests from the public and agencies. “Police have been over responding to welfare checks where there is no risk of criminality or to life or safety,” a statement read. “We are aiming to reduce demand on frontline staff but are conscious the issues are complex so we will continue to talk to partner agencies before making any final decisions.”
Police minister Mark Mitchell and minister of mental health Matt Doocey are expected to discuss the phases in years two to five with Cabinet in November.
Who will help now?
Health staff will now be considered the first responders to mental health callouts. These staffers, including those who may have already completed a full shift, will be expected to respond to after-hour callouts and to transport patients for admission with less – or zero – police assistance.
Te Whatu Ora documents obtained by Stuff last week showed standard operating procedures (SOPs) for health staff responding to mental health callouts were yet to be finalised. Interim SOPs outlined expectations before police would attend a mental health callout, including de-escalation techniques, medical or pharmaceutical intervention, using security teams or family for help, caring for a person in a low-stimulus area and removing staff and others from the area. Te Whatu Ora’s interim national clinical chief for mental health and addiction, Murray Patton, said SOPs would be finalised as the changes were rolled out and staff had given feedback.
Some health staffers take on extra responsibilities as duly authorised officers (DOAs), who are expected under the Mental Health Act to ensure required procedures are met when undertaking a compulsory assessment. A RNZ report on Monday found that at least half a dozen DOAs had forfeited their extra duties in the lead-up to the changes to the police’s response to mental health callouts because of concerns for their safety. Te Whatu Ora said this was “a very small proportion of the total number of DAOs in that area and this does not appear to be happening in other places”.
What do police and health workers think?
Police have continuously defended the decision to change their response to police callouts, with the argument that resources are being taken from criminal jobs, and that police are not always the appropriate force to respond to a mental health crisis. The Police Association has petitioned for changes in the past, and last year lobbied the government for a police response similar to the UK’s Right Care, Right Person approach to mental health, another model that has seen police reduce their response to these instances and instead treat health staff as first responders.
The New Zealand Nurses Organisation has criticised the changes, with the warning that mental health services are already over-stretched, and many nurses lack the legislative power to detain people and the tools to keep themselves safe in a crisis situation. A survey conducted by the NZNO found that 90% of respondents believed they and their patients would be more at risk without police. Another survey by the Public Service Association, mental health workers, said that nine in 10 employees also believed they and their patients would now be more at risk.
“It’s been a disaster – the police said months and months ago this was going to happen,” said NZNO chief executive Rob Goulter. “Clearly Te Whatu Ora has been so absorbed with its own internal problems that this one sailed straight past them.
“To be at the last minute still trying to sort it out at this critical juncture, when it’s a critical health and safety risk for patients as well as for staff… it’s not acceptable.”
Yesterday afternoon, Te Whatu Ora put out a statement saying it had a phased implementation plan in place, and acknowledged that “changes like these are not easy, and we recognise there will be a period of adjustment”.
“We value the work of our people throughout this transition and emphasise that we do not want staff to put themselves in risky situations,” it said. “Teams should continue to follow usual processes, including shared decision-making, seeking support of senior staff for advice, and escalating matters as needed.”
Te Whatu Ora faces its own challenges as it looks to a forecasted $1.7bn deficit by June 2025, which has been chalked up to overspending on hiring nurses, despite health workers across the motu having consistently complained about staffing and resource shortages for years. This also includes a shortage of mental health workers, an issue Te Whatu Ora plans to address with its Mental Health Workforce Plan released in September, which aims to increase the number of mental health and addiction nurses by 85% from 2025 to a total of 22 experts trained year on year.
Who else has concerns?
The Mental Health Foundation supports the concept of a health-led response, but in September wrote to police minister Mark Mitchell to express “serious concerns” about the “rapid police withdrawal”, given it had “not seen a tangible response from Health New Zealand about how the health system will be able to fill the void in acute mental health crisis presentations given unprecedented demand and the severe workforce shortages, other than a commitment “to put a robust operational plan in place”.
Sarah Gordon, an associate professor at the University of Waitako’s school of health, shared a similar sentiment in comments to the Science Media Centre, saying “an unintended result of this plan is that people experiencing mental distress may not have access to any help whatsoever. These lines in the sand for Police reducing services must correspond to others being prepared and having the ability to increase services.”